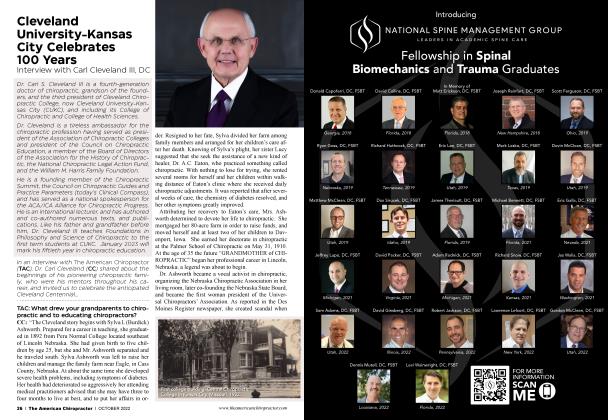
Defending Chiropractors from Predatory Insurance Carriers: Are You Next?
FEATURE
Part 1
Mark Studin
DC, FASBE(C), DAAPM, DAAMLP
I consult doctors in many healthcare disciplines, including chiropractors, neurosurgeons, head and neck surgeons, ophthalmologists, oncologists, plastic surgeons, medical primary care providers, and many others. The least favorite part of every practice, no matter the discipline, is documentation. Typically, a medical primary care provider has the most significant burden due to the scope of their evaluation. Chiropractors, although dealing primarily with the spine, are also considered a primary care provider by most licensure boards and have an increasing burden for extensive documentation.
When a doctor joins my consulting service, our first step is to do complete a compliance review, reviewing every word on every document. I create an adversarial environment where the doctor has to defend their records, and the records must speak for themselves, with no verbal explanation allowed. Regardless of the EMR [electronic medical record] used, I can say with a great degree of certainty that it is an extreme rarity that I review accurate and complete documentation. As a result, we as a profession have become an easy target to be sued for insurance fraud.
I have been reluctant to put these words on paper for over a decade. However, after reading another complaint [lawsuit] against a doctor of chiropractic claiming fraud, I am convinced the only way to resolve this issue is to shed light on it. We have for too long individually, cut too many corners in our documentation, and it is hurting our reputation as a profession. It is that reputation that will allow us to compete in the healthcare community as peers and be considered leaders in spine care.
Yesterday I had a conversation with a lawyer whose firm represents the largest insurance carriers in the nation. This lawyer confirmed the carriers consider all the issues in this article in contemporary lawsuits, as most chiropractors have the same deficiencies in their documentation. He confirmed they typically prevail, and then seek to prevent the doctor from ever billing their company again as a matter of business. The carriers contend they do not want to interact with past violators to prevent fraud going forward. For the doctor, this means you have to limit your practice going forward, even if you “cleaned up the past.” Your actions today can have lifelong consequences for your business and reputation.
When our goal is to be considered a primary spine care provider, or the first option for spine care, we need to be considered a peer to those specialists.
When was the last time you saw a “check-off’ form from a neurosurgeon, orthopedic surgeon or neurologist as their report? The answer, decades ago. As an integral part of the healthcare community, we are held to that standard. Please do not conflate my words to think I want any chiropractor to be anything other than we are. However, when our documentation is significantly inferior to a physical therapist, who often documents quite well, we are considered “second-class therapists.” When our goal is to be considered a primary spine care provider, or the first option for spine care, we need to be considered a peer. Your documentation speaks volumes to all that read it, including co-treating or collaborative providers. You read their reports, and many MD Specialists read your report, which builds your reputation, either good or bad.
Many chiropractors use handwritten or templated (a.k.a. travel cards) notes. In a Federal lawsuit (complaint) against a chiropractor, the carrier wrote, “the chiropractors at ABC Chiropractic were not creating individualized treatment plans and chart notes for each patient on each visit, but instead were using the same templated chart notes with the same Predetermined Treatment Plan for each patient. ” They continued in their complaint, “Each o f the above instances of incomplete, vague, or inaccurate chart notes viewed in an isolated claim file may appear to be a simple mistake or oversight. It is only when the claims are considered in the aggregate f6 years of combined recordsJ did a pattern emerge that ABC Chiropractic was either routinely and fraudulently charging for services that were not rendered and or were not medically necessary, or that ABC Chiropractic was improperly billing charting patient visits and treatments in violation of state law. ”
Furthermore, “ABC Chiropractic treated the 100+ adult insureds pursuant to the Predetermined Treatment to conceal its fraudulent activity, ABC Chiropractic prepared and submitted medical records designed to make it appear ABC Chiropractic was providing individualized medical care to each patient. ” The carriers argue that the templated chart only had a certain number of options, and every patient has to fit into the confines of those options, all of which lead to continued care. This supports their predetermined treatment plan argument.
The above scenario also confirms that “travelcards” should NEVER be used in a chiropractic office. They are a “prime target” for carriers, and although you might have been using one for years, look at the time-frame documented above that the carriers paid, investigated, and then demanded all of it back with interest. For argument’s sake, as too many will fight for their position and a lawsuit, you go to court, and you win. 5 years later, no sleep and $100,000’s in legal bills. Did you really win? However, chances are you will lose based upon too many before you.
A common theme is a doctor billing a 99203, but lacking the elements required in the “Expanded Problem Focused” Evaluation and Management (E&M) code. You are mandated to report chief complaint, history of present illness, and a “problem pertinent” review of systems. In my experience, 75% of doctors who bill this level of code omit the review of systems out of laziness (sorry, but true). This also holds true for many using EMR systems, where a review of systems is automated and prompts the doctor to complete the section. The answer is not to “downcode,” but to do the work. If not, you are committing fraud. In one lawsuit, the carriers wrote the following:
“Second, in some of the patient records reviewed, the patient history recorded in the chart notes did not adequately document the patient's physical condition and was insufficient to support the services billed. The histories did not include basic information relating to the patient's past medical issues (e.g., osteoarthritis, inflammatory arthritis, etc.) or current medical conditions (e.g., whether the patient was pregnant). Without this basic information, ABC Chiropractic would be unable to create an individualized treatment plan. A patient who has severe osteoarthritis inflammatory arthritis or one who is pregnant woidd certainly require a different course of treatment than a healthy young athlete. ABC Chiropractic's failure to take into account or document each patient's medical history further evidences that ABC Chiropractic was treating patients based on a Predetermined Treatment Plan and not based on the patient s specific conditions, injuries, and individualized medical needs. Additionally, without a detailed history, ABC Chiropractic could not properly bill an evaluation and management CPT code because one of the requirements of an evaluation and management code is that the physician evaluates the patient 's medical history. ”
"Grammar and accuracy matter. In approximately 80% of the documents I review, there are serious grammar issues."
The lack of documenting this basic element is indefensible when you bill a code requiring certain elements. Some contend that their initial “intake” paperwork completed by the patient has these elements. Most don’t, but for those who do, have you reviewed this with the patient, and have you documented you reviewed the paperwork? The lack thereof is grounds for a lawsuit if there is a pattern. Never forget, the carriers play the “long-game.” For argument’s sake, as too many will fight for their position and a lawsuit, you go to court, and you win. 5 years later, no sleep and $ 100,000’s in legal bills. Did you really win? However, chances are you will lose based upon too many before you.
For each region treated, you need a complaint and diagnosis that is causally related to the accident. In one lawsuit, the carrier claimed:
“Third, ABC Chiropractic 's chart notes reflect that ABC Chiropractic improperly treated at least some of its patents for injuries unrelated to the patient's motor vehicle accident, yet billed the insurance carrier for these treatments under the auspice that the injuries were related to the accident in order to unlawfully qualify for payments from the patient's No-Fault benefits. Pursuant to our state's Administrative Code § 123-45-678, an insurance company is only required to provide No-Fault coverage for medical services that are “related to the incident. ” Notwithstanding this requirement, in at least a handful of known cases, ABC Chiropractic billed the carrier for unrelated injuries. ” This is indefensible and fraudulent.
Grammar and accuracy matter. In approximately 80% of the documents I review, there are serious grammar issues. EMR notwithstanding, it is your name on the report, not a faceless programmer you might claim that created the poor grammar. It is your reputation on the line, and worse, poor grammar can change the context of your findings. Read your reports. Close to 0% of the doctors I do a compliance review with proof their reports. Here is what inaccuracy leads to in a recent lawsuit:
“Fourth, there were several instances wherein the medical records mixed-up patient names. The name mix-ups continued from chart note to chart note for several months evidencing that the chiropractors at ABC Chiropractic were not creating individualized treatment plans and chart notes for each patient on each visit, but instead were using the same templated chart notes with the same Pre-determined Treatment Plan for each patient. ”
The lawsuit continued, “Each of the above instances of incomplete, vague, or inaccurate chart notes viewed in an isolated claim file may appear to be a simple mistake or oversight. It is only when the claims are considered in the aggregate did a pattern emerge that ABC Chiropractic was either routinely and fraudulently charging for services that were not rendered and or were not medically necessary, or that ABC Chiropractic was improperly billing charting patient visits and treatments in violation of state law. ”
Unlike other consultants who help you build your practice, I do not care if you make another dime as my first priority. My primary concern is compliance, and I don’t want you to have to give it all back. If there is a pattern of fraud, you can be exposed to RICO charges and will then have to give back three-fold, as per the law if found guilty. We start with compliance as that is the foundation of all practices, and too many overlook the obvious. Getting patients and making money is comparatively easy; keeping the money is too often challenging. The purpose of this article is not to say, “the sky is falling; it is to say Caveat Emporer. Many doctors are defending their documentation while the carriers are successfully useing fraud as a profit center. They will go after either the largest offices or the easiest targets based upon insufficient documentation. You don’t hear much from friends about being sued. If you were being sued, would you tell everyone? The answer is no. However, because of my position in the chiropractic industry, I am often sought out for counseling or retained to help defend doctors, and I get to see the stark truth of your documentation. The equation is simple; when it comes to compliance, you either get to see what your documents are either doing FOR you or TO you.
This is the first article of a 4-part series. In part 2 of this series, I will be joined by many others in academia, and will uncover what the carriers consider predetermined treatment plans and what modifications are required in your documentation to avoid that allegation. Also, we will uncover how the carriers aggregate statistics of your care to be used against you. Lastly, we will delve into the necessary documentation for x-rays utilization. This is required to overcome both the carrier’s “apparent” financially motivated allegations and the American Chiropractic Association’s documented influence in legal cases against chiropractors.
Mark Studin, DC, FASBE(C), DAAPM, DAAMLP, has been a practicing chiropractor since 1981. He teaches various subjects (www. TeachDoctors.com), ranging from MRI Interpretation, Concussion, Stroke, Spinal Biomechanics, Triaging the injured, etc. at various levels through both chiropractic and medical academia. He also coordinates a clinical rotation for chiropractic students in Neuroradiology at the State University of New York at Stony Brook, School of Medicine. He is the president of the Academy of Chiropractic, teaching doctors of chiropractic how to interface with the medical and legal communities (www.DoctorsPIProgram.com). Reach Dr. Studin at: DrMark@ AcademyofChiropractic.com or at 631-786-4253.
 View Full Issue
View Full Issue