Did You Know?
In our modern age, the average newborn baby has over 287 known toxins in his or her umbilical cord. As a population, we are exposed to 6 million pounds of mercury and 2.5 billion pounds of other toxic chemicals each year. An estimated 80,000 toxic chemicals have been released into our environment since the dawn of the industrial revolution, with very few of them having been tested for their long-term impact on human health. We certainly are not experiencing the fresh country living of our forefathers.
The long-term effects of these combined toxins are still being fully weighed. However, we do know that in this modern age (within the last five decades, really), people have not become healthier. Our populace suffers from more chronic disease and autoimmune issues than ever before, to the point that experts have even termed it a “twenty-first-century chronic disease epidemic.” It makes us strongly consider the possible correlations between our exposures and the new preponderance of disease.
Why are some of us more affected by exposures while others seem to handle the toxic load better, seemingly with no effects? The answer includes our unique genetic and biochemical individuality. The properly functioning human body has one heck of a detoxification system, but a properly functioning human body is what's key.
In this next series of articles, we will visit the concepts of detoxification. Detox is an oversimplified catchphrase in media that could mean anything from a special diet to super powders and vitamin protocols, all looking to clear unwanted substances from the body. First, though, a patient's detoxification/ biotransformation system must be working as it was designed. As we decode detox in this series, we are going to look at the physiological processes surrounding detox in the body and what causes issues in the mechanics of those processes.
Phases of Detox
There are two phases for basic detox processes in the body, as well as an antiporter system that some refer to as phase three. In a nutshell, phases one and two work to biochemically transform toxic substances into progressively more water-soluble substances that can be more easily excreted. This happens in the liver, the intestinal mucosal wall, and the kidneys.
Phase one: Includes reactions like oxidation, reduction, hydrolysis, hydration, and dehalogenation. These reactions are based on the cytochrome P450 enzymes. This phase is, in general, the first enzymatic defense we have against foreign compounds (xenobiotics, petrochemical hydrocarbons, many medications, or endogenous steroid hormones/products that could become toxic if allowed to accumulate.) We are oversimplifying the process for review, but please remember that this phase includes several hundred identified variations of isoenzymes and substrates. Phase one works to transform toxins into intermediate substances, and harmful free radicals are formed from this activity.
Phase two: Serves to neutralize radicals or transform them into harmless molecules like water. That is accomplished by antioxidant activity, so it is crucial to have ample amounts of antioxidants in the diet for this process. The process includes conjugation pathways and processes, such as sulfation, glucuronidation, glutathione conjugation, acetylation, amino acid conjugation, and methylation. Phase one prepares substances to enter this phase. In most cases, these reactions are working to decrease the biological activity/toxicity of the parent molecule that is being received, e.g., the intermediate metabolites created in phase one. The chemical structures are striving to combine with hydrophilic compounds with the goal of rapid excretion from the body. Conjugate reactions occur with a variety of substances and involve cofactors, which are derived from metabolism. The final goal is for the derivatives to be excreted into the bile (to land in the feces) or the serum (to move to the kidneys/urine)
Antiporter System: The transport of hydrophilic metabolites out of hepatocytes in the liver after phase two is referred to as phase three, or the antiporter system. An antiporter is a membrane transport protein that moves substances across a phospholipid membrane. Antiporter efflux is also utilized in phases one and two. The antiporter role has been increasingly studied because of its dual functions of transportation of conjugated metabolites after phase two and the elimination of toxins before biotransformation (prepping for excretion). This makes antiporter activity a crucial factor in the first pass metabolism of pharmaceuticals and other xenobiotics.
Clinical Note: Sometimes intermediate substances created during the detox breakdown can be more toxic than the initial substance. It is crucial that all phases of detox are balanced and adequately supported to do their job. This also includes assimilation/gut health so that toxins are not reabsorbed and are promptly excreted.
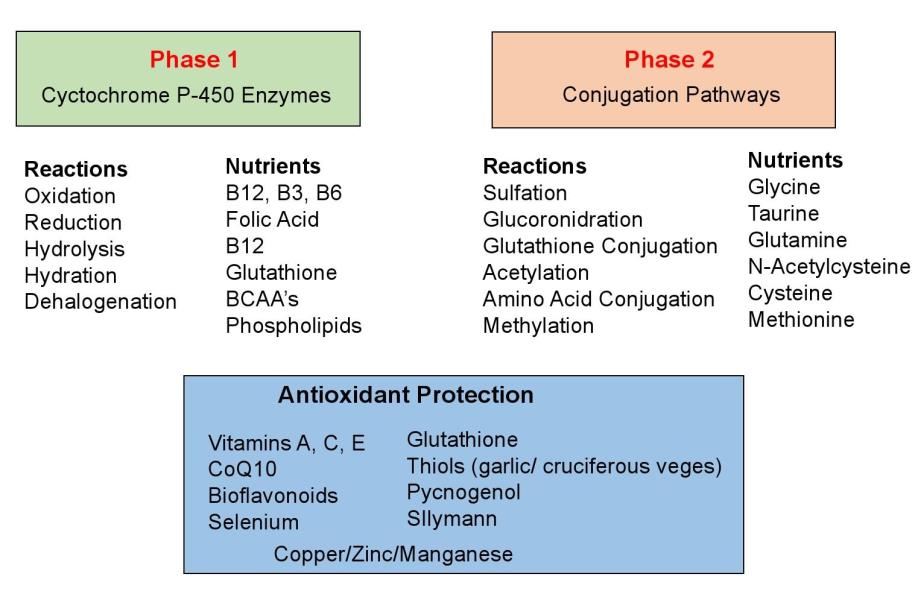 Image 2
Image 2
What Can Happen if Detox Phases Are not in Working Order?
Once the exported unwanted compound returns to the intestine, one of several things can take place, some desired, others not:
Unhealthy GI function can allow toxins and other harmful chemicals to leak through the compromised intestinal wall and flow to the liver. In an unhealthy liver, phase one toxins may not be completely transformed, and, in turn, intermediates may not be completely transformed by phase two enzymes. In an unhealthy liver, toxins may leave the liver unchanged and then can be stored in tissues, such as fat and the brain/nervous system. These stored toxins have the potential to recirculate in the blood and contribute to long-term health issues. For example, heavy metals have been linked to damaging effects on the brain, such as encephalopathy and dementia.
Supporting and Balancing Detox Phases
Phase one and phase two must be functioning in proper balance to successfully complete the detoxification process. This is really a key point to understand. As stated previously, keep in mind that the reactive intermediate metabolites produced during a phase of the process may actually be more harmful or toxic than the original substance. We must complete the full process to rid the body of the toxins, which means our GI system must be healthy and functioning properly.
Other endogenous molecules involved in cellular communication can also be compromised if detox function is not working properly. Imbalance can influence the amounts and types of steroids produced as well as fatty acids. Less tissue damage and less stress from oxidants and free radical generation occur when reactive intermediates are promptly acted upon by a phase two reaction, completing the process.
As patients strive to detox efficiently, specific nutrients need to be in place to support these phases (along with a healthy GI). The chart we’ve created provides a good basic outline of nutrients needed for specific reactions to occur. Note that antioxidant protection is required for all reactions, and antioxidant intake cannot be underestimated.
Next Time
Now that we’ve laid a foundation, the second part of this series will look closer at the different elements of toxic load, where we tend to find them in our daily lives, and how to strive to eliminate them in our patients and their daily living.
Laurie Mueller, BA, DC, CFMP, served in private practice in San Diego, California. She served as the ACC postgraduate subcommittee chair for six years, peer-reviewed for the Research Agenda Conference, and was the postgraduate director for the Palmer Colleges from 2000 to 2010. Dr. Mueller currently works as a private eLearning consultant with a focus on healthcare topics and functional medicine through her company, Impact Writing Solutions, LLC. She partners with companies and organizations to launch/administer eLearning initiatives, and she is also the founder of www.cccaonline.com for CAs and www.FxMedOnline.com for allied health professionals. TAC readers can enjoy $10 off their first registration bundle by utilizing TAC's exclusive discount code at the time of purchase—TACFXMED.
References:
1. Altern Ther Health Med. 2007 Mar-Apr;13(2): S108-11. Diet, genetic polymorphisms, detoxification, and health risks.Lampe JW.
2. http://www.fxmedicine.com.au/b...
3. Liska DJ. The detoxification enzyme systems. Alt Med Rev 1998;3(3):187-198.
4. Textbook of Functional Medicine. IFM 2010 p.275-298.
5. https://www.dementia.org/demen...
6. J Environ Public Health. 2012; 2012: 184745.
7. Published online 2012 Feb 22. PMCID: PMC3312275
 View Full Issue
View Full Issue