Our last article reviewed the three phases of detoxification in the body and how to support them. As a reminder, before starting any sort of detox protocol, we want to ensure that gut function/assimilation is fully intact to do its job in the process. In this article, we will review how to determine the toxic load in the body and the source of many common toxins.
Determining Toxic Load
How do you determine the toxic load in a patient? Toxic load translates to the amount of toxins that your body must process. Think about food choices, external toxins or exposures, endotoxins created in the body, and emotions that lead to stress. As practitioners, you may find that beginning with a short questionnaire to provide a snapshot of patient habits can be helpful. Examples of basic questions to get patients thinking may include questions such as:
• Do you eat processed or whole foods?
• Do you eat non-organic fruits, vegetables, or meat?
• Do you use or have you ever used artificial sweeteners?
• Do you drink soda?
• Do the foods you eat have preservatives, additives, dyes, or sweeteners added?
• Do you eat more whole foods or fast foods?
• Do you drink alcohol?
• Do you drink tap water or filtered?
• Do you wash all of your produce? (Note that it is a common misconception that organic produce is pesticide-free or doesn't need washing, but it is prudent to wash all fruits and vegetables.)
Those are just examples. From a healthcare standpoint, a questionnaire that is much more comprehensive and includes details about what they eat (food diary) and external toxins, such as personal care products, cleaners, pollution, or other exposures (e.g., mercury fillings, farming chemicals, hair chemicals), should also be included in a complete history. Also, don’t forget that emotions, such as anger, fear, helplessness, and sadness (stress), can also affect our detoxification functions, so emotional/spiritual health comes into play here and may need to be addressed.
Where do we Find Common Toxins?
Coming from the outside, we should be cognizant of a variety of sources:
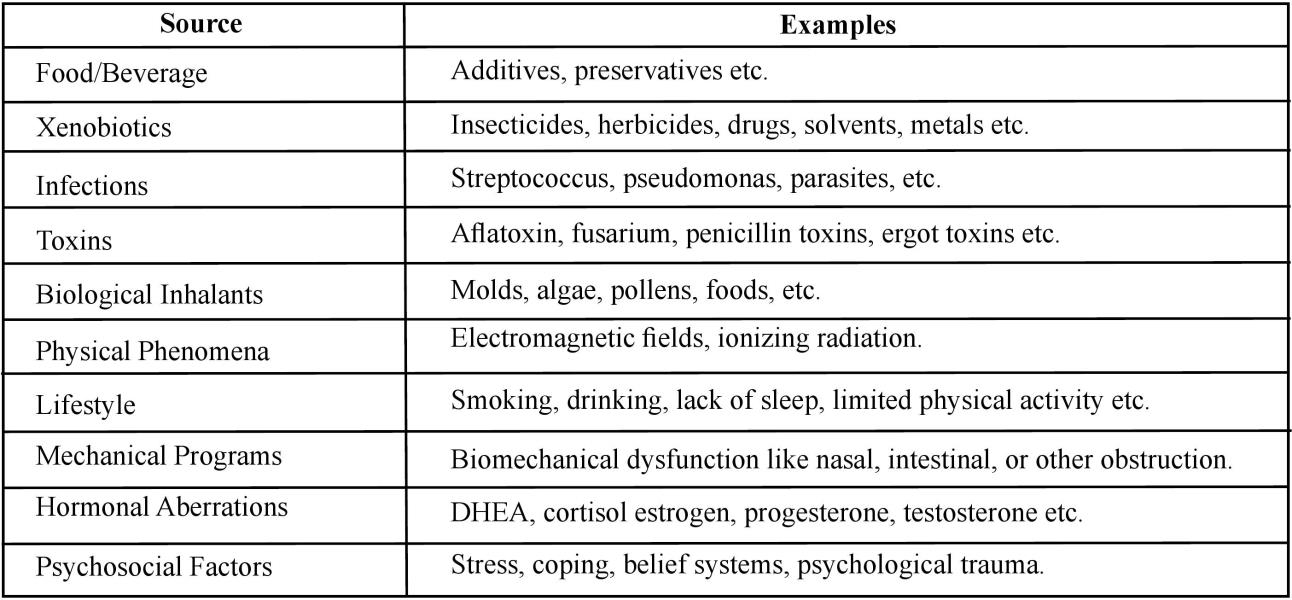
That shows us broad-stroke sources. Next, we want to outline some very common household toxins that can add up to toxic load. How many of these things are you and your family exposed to every single day?
Triclosan: An antibacterial agent that is chemically similar to the dioxin class of compounds.
Phthalates: Large phthalates are chemicals added to plastics to impart resilience and flexibility. Smaller phthalates are used to prolong the length of time that a scented product maintains its fragrance.
Bisphenol A: Used in epoxy resins that line some metal cans and to make polycarbonate plastics utilized in a variety of food containers and baby products.
Carbon monoxide: Lormed from incomplete combustion of fuel. Carbon monoxide decreases the delivery of oxygen to cells.
Perfluorinated chemicals: Used to make stain repellents and nonstick surfaces.
Volatile organic compounds (VOCs): Chemicals released into the air as gases.
Radon: Odorless gas that forms as uranium in rocks and soil breaks down.
Lead: A heavy metal that can build up in our tissues.
Pesticides and herbicides: Linked to problems with the nervous system and possibly a risk factor for cancer, developmental challenges, and reproductive problems.
Halides: Endocrine disruptors commonly found in toothpaste (fluoride), brominated flour (bromide), and municipal H20.
Knowing where to find these elements gives patients a better chance of eliminating them in daily living. In our longer course, we also cover the correlations between these elements and autoimmune conditions as well as conditions with cognitive decline.
Testing
Along with a thorough history that creates a timeline picture of possible exposure points and symptoms that might point to detox issues, several labs and assessments can help us test for toxins and detoxification function. We are not going to name specific lab companies, but a variety of them exist that can run toxicant panels to provide you with more information for “the big picture” with your patients. That could include things such as challenge testing, detox enzymes, genetics, heavy metals, organic acids, and a variety of other considerations.
Standard liver function tests can certainly provide a measure of hepatic damage (released hepatic enzyme levels). However, you may choose to further evaluate liver detoxification with functional testing that looks at the ability of an individual to process substances such as caffeine, aspirin (salicylate), and paracetamol (acetaminophen) by assessing certain metabolites in salivary and urinary specimens. Such testing will obtain specific measurements of the different phases of liver detoxification, including phase I and phase II (glycation, glucuronidation, sulphation, and glutathionation). Those results can then aid in guiding the design of effective and specific therapeutic strategies, which can optimize liver function.
Tests that assess the liver's detox function can have various names depending on the lab—expect “functional liver challenge tests” or “functional liver detoxification profile.” We can also look to conventional labs tests for early Indicators of toxic exposure to select substances. Pizzorno reminds us, “Except for CBC and platelet count, we really want our patients in the lowest quartile of the range for these tests.” The following list contains possible toxic causes for lab results:
• WBC/platelets at the bottom edge of normal? (solvents, PCBs, OCPs)
• Basophilic stippling of RBCs? (arsenic and lead)
• Fiver enzyme GGTP elevated? (toxic metals and POPs)
• Inflammatory markers increased? (most environmental toxins)
• Fipid increase? (select PCBs and POPs)
• Metabolites increased? (PFOA and PFOS body load)
• Bilirubin increased? (PCBs)
• Blood sugar regulation issues? (general toxic load/ insulin binding site competitors)
Functional practitioners may also look at detoxification enzymes, genetic correlations for detox, chemical antibody testing, or organic acid testing in the urine to paint a larger picture.
Detox Strategies
A variety of strategies can aid in reducing toxic load with patients. We’ve mentioned diet, lifestyle choices, and GI function. For some patients, you will want to consider a detoxification process, also called a purification protocol. Such a plan may include more profound dietary changes, supplementation with vitamins/minerals, and specific detoxification products that will aid in releasing toxins from the tissues where they have accumulated.
Before going forth with a plan to release toxins, it is important to ensure that the phases of detox are in order and that the patient’s other systems are working well (assimilation) so that they can excrete the toxins properly. It is vital that the patient is healthy enough to tolerate the processes of clearing the toxins. Also, be very aware that obese patients may have a harder time because toxins can be stored in fat cells, so their toxic load will increase as fat breaks down.
Detoxing is certainly a full course all by itself. A good start for all patients includes helping your patients remove the found toxic substances from their living and working areas so they don’t continue to be exposed. Patients should eat foods that support detox, such as cruciferous vegetables, garlic, green tea, water, antioxidants, high-quality sulfur contain proteins, and flavonoids. They also may need to supplement with vitamin C, EFAs, N-acetylcysteine amino acids, and bioflavonoids.
Finally, if you perform organic acid testing, you can further correlate what potential nutritional interventions may work best with the oxidative damage markers that you find.
Laurie Mueller, BA, DC, CFMP, served in private practice in San Diego, California. She served as the ACC postgraduate subcommittee chair for six years, peer-reviewed for the Research Agenda Conference, and was the postgraduate director for the Palmer Colleges from 2000 to 2010. Dr. Mueller currently works as a private eLearning consultant with a focus on healthcare topics and functional medicine through her company, Impact Writing Solutions, LLC. She partners with companies and organizations to launch/administer eLearning initiatives, and she is also the founder of www. cccaonline.com for CAs and www.FxMedOnline.com for allied health professionals. TAC readers can enjoy $10 off their first registration bundle by utilizing TAC's exclusive discount code at the time of purchase—TACFXMED.
References:
1. The World Incidence and Prevalence of Autoimmune Diseases is Increasing
2. Aaron Lernerl,, Patricia Jeremias2, Torsten Matthias2
3. International Journal of Celiac Disease Vol. 3, No. 4, 2015, pp 151-155. doi:10.12691/ijcd-3-4-8 I Research Article
4. https://www.gdx.net/core/one-p...
5. Pastore, Anna; Piemonte, Fiorella; Locatelli, Mattia; To Russo, Anna To; Gaeta, Laura Maria; Tozzi, Giulia; Federici, Giorgio (August 2001). "Determination of blood total, reduced, and oxidized glutathione in pediatric subjects". Clinical Chemistry. 47 (8): 1467-9. PM1D 11468240.
6. Methods Mol Biol. 2010;603:423-31. doi:10.1007/978-160761-459-3_41.
7. Urine organic acid analysis for inherited metabolic disease using gas chromatography-mass spectrometry.
8. Jones PM1, Bennett MJ.
9. www.drbenkim.com/articles-hous...
10. JNutrMetab. 2015; 2015: 760689.
11. Published online 2015 Jim 16. doi: 10.1155/2015/760689
12. PMC1D: PMC4488002
13. Modulation of Metabolic Detoxification Pathways Using Foods and Food-Derived Components: A Scientific Review with Clinical Application
14. Romilly E. Hodges 1 and Deanna M. Minich 2,3,*
15. Altern Tlier Health Med. 2015 May-Jun;21(3):54-62.
16. Nutritional aspects of detoxification in clinical practice .
17. Cline JC.
18. The MSDS HyperGlossary: Acute toxicity". Safety Emporium. Archived from the original on 16 October 2006. Retrieved 200611-15.
19. IUPAC, Compendium of Chemical Terminology, 2nd ed. (the "Gold Book") (1997). Online corrected version: (2006-) "acute toxicity
20. http://www.atsdr.cdc.gov/csem/...
 View Full Issue
View Full Issue