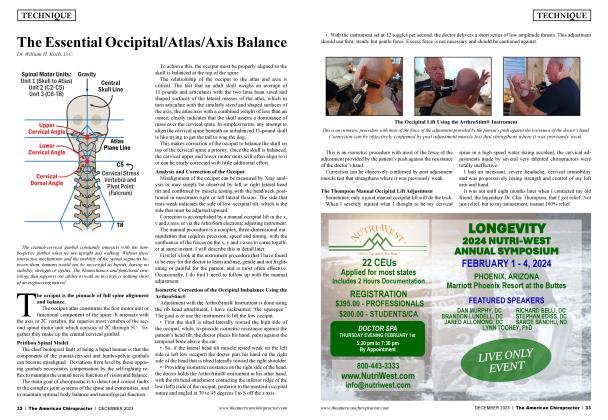
Tethers, Torsion, and Tension
FEATURE
The Myofascial Conundrum
Dr. Monica Buerger
“A fundamental characteristic of the fascia is the ability to adapt to mechanical stress...”
DESPITE SCIENTIFIC UNCERTAINTY, there is an agreement within medical literature that the fascia covers every structure of the body, creating a structural continuity that gives form and function to every tissue and organ. The fascial system has a ubiquitous distribution in the body; it wraps, interpenetrates, supports, and forms the bloodstream, bone tissue, meningeal tissue, organs, and skeletal muscles. The fascia creates different interdependent layers with several depths, from the skin to the periosteum, forming a three-dimensional mechano-metabolic structure1 that extends from the cranium to the toes.
Interoception, Fascia, and Mood
Interoception constitutes the interior dialogue between your body and your nervous system, establishing a person’s ‘‘sense of self.” The perception and integration of joint movement (proprioception), head movement (vestibular), and autonomic, hormonal, visceral, and immunological homeostatic signals collectively describe the physiological state of the body. Interoceptive pathways project to the autonomic and homoeostatic centers and the brainstem. From there, they project to the anterior cingulate cortex (ACC) and the dorsal posterior insula by way of the thalamocortical circuit.3
The emotional or affective pain experience is largely processed in the ACC. Chronic pain syndromes often associated with hypervigilant interoceptive awareness are associated with altered ACC responses to nociception. The ACC is also highly associated with mood disorders and anxiety. The role of the dorsal posterior insula appears to be responsible for the recognition, intensity encoding, localization, learning, and memory of somatically painful events.4
The interconnectivity between the fascia and the entire body can be viewed like a marionette puppet; when you pull the string on the left arm, the right big toe moves. The connections are not linear in nature and can create tethering, tension, torsion, and neuromechanical restrictions anywhere in the body. That is why it is so important to look at the body as a dynamic system rather than being hyperfocused on the specific region of reported pain. The fascia plays different physiological and functional roles related to joint stability, general movement coordination, proprioception, and nociception.2
Unmyelinated C-tactile fibers lie in the myofascial continuum. Through C-tactile afferent fibers, the myofascial system stimulates areas of the brain, such as the ACC and dorsal posterior insula, which deal with chronic pain, mood, and emotional states. Theoretically, emotional allodynia could originate from constant myofascial nonphysiological afferents, which would bring the emotional state and the myofascial pathology to the same level. Myofascial restrictions lead to biomechanical dysfunction and postural alterations. It is known that the position of the body stimulates the areas of emotionality.5
Previous embodiment findings indicate a relationship between physical posture and mood, suggesting upright postures induce positive mood states. Findings also showed a relationship between moods and cognitive performance. While positive mood states were found to be related to increased processing speed, negative mood states were associated with higher processing accuracy in cognitive task performance.6 Higher processing accuracy can be associated with hypervigilant interoceptive awareness and lower pain thresholds.
The term body feedback describes feedback from the entire body, during which information is transferred from the body to the brain and, thus, to the cognitive and psychological processing system.7 Therefore, it is important not to view the fascial system solely from a point of restricted movement but also from a brain, cognition, mood, and psychological perspective.
Neuromechanical Restrictions from Bottom Up
Normal movement of the body is allowed because of the presence of fascial tissues and their inseparable interconnection, which allow the sliding of the muscular structure, the sliding of nerves and vessels between contractile fields and joints, and the ability of all organs to slide and move with each other as influenced by the position of the body.
Afundamental characteristic of the fascia is the ability to adapt to mechanical stress, remodeling the cellular/tissue structure and mirroring the functional necessity of the environment where the tissue lies. For example, the plantar fascia in the foot adopts a mechanical model known as the “windlass mechanism” to provide dynamic support for the medial longitudinal arch while the limb transitions from the heel strike to toe-off phases of the gait cycle.8 The windlass mechanism describes how the plantar fascia supports the foot during weight-bearing activities and provide information about the biomechanical stresses placed on the plantar fascia.
Studies over the past 20 years have revealed that there are fibrous connective tissues between the suboccipital muscles, nuchal ligament, and cervical spinal dura mater (SDM). This fibrous connection with the SDM is through the posterior atlanto-occipital or atlantoaxial interspaces, called the myodural bridge (MDB).9
Soft tissue communications linking suboccipital muscle fascia and the dura and its role in cervical neuromuscular control have been more recently studied. These myodural bridges have been associated with the etiology of cervicocephalic headaches and cervicocephalic pain syndromes. These epidural connections may also be involved passively as a dural anchor and an active stabilizer of the spinal cord.10
Viewing the body from a dynamic systems approach, myofascial restrictions create tethering and tension along the continuum from the cranium to the feet. These myofascial restrictions can lead to chronic vertebral subluxation patterns. Likewise, vertebral subluxations can lead to chronic myofascial restrictions. Putting this information into practical context, we can understand why chiropractic care has been associated with patient reports of a healthier sense of being, a more positive mood, and decreased pain.
Management Considerations
Knowing that the fascial system is rich in interoceptive input into the brain and plays a large role in chronic pain, mood, and emotional well-being, it is important for the practicing chiropractor to understand the best management approach to use for each patient. Along with specific chiropractic adjustments, myofascial release techniques, cranial-sacral techniques, stretching, and visceral-release techniques should be considered, especially for those reporting chronic pain syndromes.
Providing custom flexible three-arch orthotics that allow for optimal functional support of foot mechanics and align, balance, and stabilize the entire body is another important consideration. Low-level laser, dry needling, and red-light therapy are also beneficial for myofascial restrictions and fascial pain syndromes.
References
Dr. Monika Buerger, a 1991 Life Chiropractic College West graduate, is the owner of Eagle Canyon Wellness & Sensory Development Center in Ammon, Idaho. She is a teacher, international lecturer, author, and the founder of lntersect4Life Educational Seminars and developingMINDS certification program in childhood and adolescent neurodevelopment. For additional information, visit www. intersect4life.com and www.devmindsu.com.
1. Bordoni B, Marelli F, Morabito B, Sacconi B. The indeterminable resilience of the fascial system. J IntegrMed. 2017 Sep;15(5):337-343. doi: 10.1016/S2095-4964( 17)60351-0. PMID: 28844209.
2. Tozzi P. Selected fascial aspects of osteopathic practice. J Bodyw Mov Ther. 2012 Oct;16(4):503-19. doi: 10.1016/j.jbmt.2012.02.003. Epub 2012 Feb 26. PMID: 23036882.
3. Tsay A, Allen TJ, Proske U, Giummarra MJ. Sensing the body in chronic pain: a review of psychophysical studies implicating altered body representation. Neurosci Biobehav Rev. 2015 May;52:221-32. doi: 10.1016/j.neubiorev.2015.03.004. Epub 2015 Mar 14. PMID: 25783221.
4. Coen SJ, Hobson AR, Aziz Q. Chapter 23: Processing of Gastrointestinal Sensory Signals in the Brain. In: Johnson LR, Ghishan FK, Kaunitz JD, Merchant JL, Said HM, Wood JD. Physiology of the Gastrointestinal Tract (Fifth Edition). Academic Press; 2012. p. 689-702.
5. Bordoni B, Marelli F. [Emotions in Motion: Myofascial Interoception]. Complement Med Res. 2017;24(2): 110-113. German, doi: 10.1159/000464149. Epub 2017 Mar 10. PMID: 28278494.
6. Awad S, Debatin T, Ziegler A. Embodiment: I sat, I felt, I performed — Posture effects on mood and cognitive performance. Acta Psychol (Amst). 2021 Jul;218:103353. doi: 10.1016/j.actpsy.2021.103353. Epub 2021 Jun 16. PMID: 34146977.
7. Koch SC. Rhythm is it: effects of dynamic body feedback on affect and attitudes. Front Psychol. 2014 Jim 10;5:537. doi: 10.3389/ fpsyg.2014.00537. PMID: 24959153; PMCID: PMC4051267.
8. Bourne M, Talkad A, Varacallo M. Anatomy, Bony Pelvis and Lower Limb, Foot Fascia. 2023 Aug 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. PMID: 30252299.
9. Zheng N, Chi YY, Yang XH, Wang NX, Li YL, Ge YY, Zhang LX, Liu TY, Yuan XY, Yu SB, Sui HJ. Orientation and property of fibers of the myodural bridge in humans. Spine J. 2018 Jun;18(6):1081-1087. doi: 10.1016/j.spinee.2018.02.006. Epub 2018 Mar 15. PMID: 29477753.
10. Enix DE, Scab F, Pontell ME. The cervical myodural bridge, a review of literature and clinical implications. J Can Chiropr Assoc. 2014 Jun;58(2):184-92. PMID: 24932022; PMCID: PMC4025088.
 View Full Issue
View Full Issue