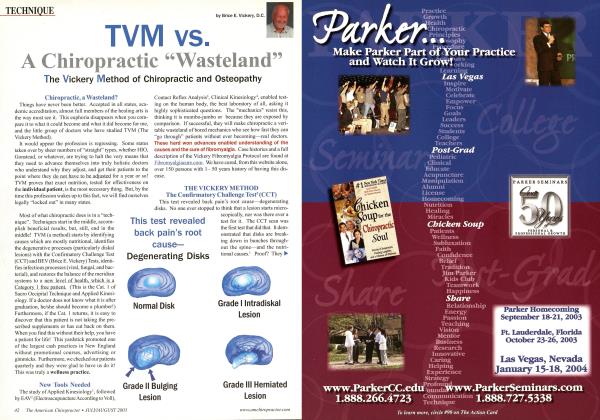
Below are X-rays of different patients who have sustained trauma to the lumbar spine. The two most common fractures in the lumbar spine are demonstrated in the figures below. Can you identify them? C ompression fractures are the most common fractures of the lumbar spine. They result from combined flexion and axial compression.'-: The most common segmental levels to develop compression fractures are T12-L1/ The extent of the vertebral compression and degree of comminution are dependent upon the severity of the force applied and the relative strength of the vertebra.4 In children, they are torus-type fractures. In the elderly, osteoporosis can precipitate spontaneous compression fractures during everyday activities, which technically render them classifiable as insufficiency fractures ("grandma fractures"). Up to 35% of compression fractures in female patients over the age of forty-five years may be due to early menopause and 30% to secondary osteopenia, most often from corticosteroids (15%), hyperthyroidism (8%), and malignancy (less than 2%).5 The disruption of the cortical vertebral endplate causes acute symptoms of only ten-to-four-teen days, duration, as long as no dislocations accompany the fracture.6 Post-fracture stability is determined based on the classification by Denis.7 Three columns are recognized: anterior column (from the anterior longitudinal ligament to the midvertebral body), middle column (from the midvertebral body to the posterior longitudinal ligament), and the posterior column (from the posterior longitudinal ligament to the supraspinous ligament). If two or more compartments are disrupted, the fracture complex is unstable. The likelihood of neurologic injury is high and interventional surgery is likely to be necessary. Continues ► ^...from Page 12 Radiographic Signs of Vertebral Compression Fracture Radiographs of optimum quality are necessary in order to adequately demonstrate these fractures. Lateral radiographs best demonstrate fracture features. Radiographic signs of vertebral compression fracture include a step defect, wedge deformity, linear zone of condensation, and displaced endplate. The Step Defect Since the anterior aspect of the vertebral body is under the greatest stress, the first bony injury to occur is a buckling of the anterior cortex, usually near the superior vertebral endplate. This sign is best seen on the lateral view as a sharp step-off of the anterosuperior vertebral margin along the smooth concave edge of the vertebral body. In subtle compression fractures, the "step" defect may be the only radiographic sign of fracture. Anatomically, the actual step-off deformity represents the anteriorly displaced corner of the superior vertebral cortex. As the superior endplate is compressed in flexion, a sliding forward of the vertebral endplate occurs, creating the roentgen sign. Wedge Deformity In most compression fractures, an anterior depression of the vertebral body occurs, creating a triangular wedge shape. The posterior vertebral height remains uncompromised, differentiating a traumatic fracture from a pathologic fracture. This wedging may create angular kyphosis in the adjacent area. The superior endplate is far more often involved than the inferior endplate. Up to 30% or greater loss in anterior height may be required before the deformity is readily apparent on conventional lateral radiographs of the spine.s Normal variant anterior wedging of 10-to-15%, or 1 -3 mm, is common throughout the thoracic spine most marked at T11-L2.910 In all compression fractures, there should be clear differentiation from an underlying pathology that has produced the fracture. Key features of pathologic fractures may be identified by loss of the posterior body height, pedicle, and other sites of destruction. A paraspinal mass on MR imaging with abnormal marrow can be demonstrated.'' Linear White Band of Condensation (Zone of Impaction) Occasionally, a band of radiopacity may be seen just below the vertebral endplate that has been fractured. The radiopaque band represents the early site of bone impaction following a forceful flexion injury where the bones are driven together. Callus formation adds to the density of the radiopaque band later, in the healing stage of the fracture injury. This radiographic sign is striking when present; however, it is an unreliable sign, since it is not present as often as might be expected. Its presence, however, denotes a fracture of recent origin (less than two months' duration). It is nicely demonstrated in Figure 1. (See page 12) Disruption in the Vertebral Endplate A sharp disruption in the fractured vertebral endplate may be seen with spinal compression fracture. This may be difficult to perceive on plain films and tomography; CT (computed tomography) provides the definitive means to identification. The edges of the disruption are often jagged and irregular. The superior endplate is more commonly fractured than the inferior endplate. Transverse Process Fractures Transverse process fractures are the second most common fractures of the lumbar spine, with compression fracture being the most common. They occur, usually, secondary to a severe hyperextension and lateral flexion blow to the lumbar spine from avulsion of the paraspinal muscles. The most common segments to suffer transverse process fractures are L2 and L3. Radiographically, the fracture line appears as a jagged radi-olucent separation, usually occurring close to its point of origin from the vertebra. Frequently, the separated fragment is displaced inferiorly. If the fracture line is horizontal, close inspection for a transverse or Chance fracture should be performed. Fractures often occur at multiple levels. Fractures of the fifth lumbar transverse process are frequently found in association with pelvic fractures, particularly fractures of the sacral ala, or disruption of the sacroiliac joint. Occasionally, loss of the psoas shadow may occur secondary to hemorrhage. Ossification within the hemorrhage (myositis ossificans) can result in bony bridging between transverse processes (lumbar ossified bridging syndrome, LOBS).12 Renal damage may occur which may be associated with hematuria. A pseudofracture of the transverse process can be simulated by developmental nonunion, especially at LI, the psoas margin where it crosses the tip of the transverse process and overlying fat lines, or intestinal gas. Oblique or tilt views may be necessary to rule out fracture.11 See References on Page 59 Dr. Terry R. Yochum is a second-generation chiropractor and a cum laude graduate of the National College of Chiropractic, where he subsequently completed Ms radiology specialty. He is currently Director of the Rocky Mountain Chiropractic Radiological Center, in Denver, CO, an Adjunct Professor of Radiology at the Los Angeles College of Chiropractic, as well as an instructor of Skeletal Radiology at the University of Colorado School of Medicine, Denver, CO. Dr. Yochum is, also, a consultant to Health Care Manufacturing Company that offers a Stored Energy system. For more information. Dr. Yochum can be reached at: (303) 940-9400 or by e-mail at dcradQ99%aol.com. Dr. Chad Maola is a 1999 Magna Cum Laude Graduate from National College of Chiropractic. TAC's MISSION: We are dedicated to the continuing education & advancement of the chiropractic professional—YOU! Figure 1. Compression Fracture of the L1 Vertebral Body. Observe the linear white band of condensation (zone of impaction) seen throughout the mid vertebral body. This is a positive radiographic sign for vertebral compression fracture, along with the wedge-shaped vertebral body. Figure 2. Transverse Process fractures of L1, L2 and L3. Note the transverse process fractures on the left side of the L1, L2 and L3. Dr. Terry R. Yochum Dr. Chad Maola
 View Full Issue
View Full Issue