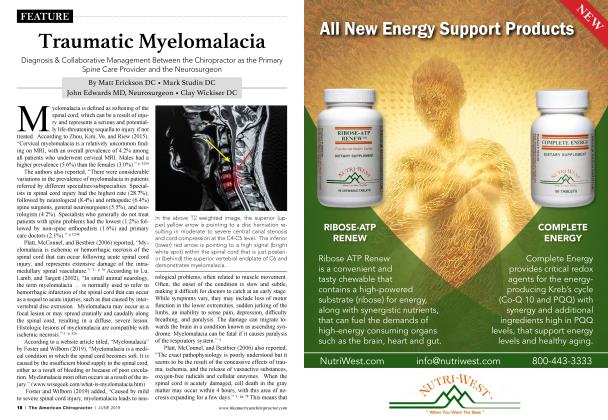
The Neurodynamic Consequences of Chronic Spinal Misalignment
SUBLUXATION
Dr. William H. Koch
The chiropractic profession has saddled itself for too long with an antiquated and cliched description of the vertebral subluxation and mechanisms of nerve interference. Such simplistic explanations do not serve us well and create an immediate credibility gap with other healthcare professionals and anyone educated in the basic sciences.
Fortunately, there are scientifically valid descriptions of the subluxation complex and the mechanisms of neurological interference.
It is important for us individually and as a profession that the vertebral subluxation complex and resultant neurophysiological consequences are described accurately and in valid scientific terms. Likewise, the chiropractic corrective procedures widely known as the chiropractic adjustment should be described in scientifically valid terms and employed to achieve an equally scientifically valid and definable objective.
I subscribe to a fundamental principle of mechanics that you cannot fix anything unless you first understand how it works. This is true of the human spine functioning under the force of gravity just as it is for any other complex mechanical system.
We as chiropractors are fortunate in that our art and science allow us the opportunity to directly apply the sciences of physics, mathematics and the principles of mechanical engineering to our clinical practices.
The principles of Spinal Biomechanical Engineering I am sharing here were pioneered by my friend, teacher, and mentor, Dr. Burl Pettibon, who I am sad to report passed away on December 22, 2017. In his research program that spanned 60 years he employed the services of engineers, physicists, mathematicians, and even NASA scientists to help him understand the complexities of the human spine. Working together with Dr. Pettibon and the associates of the Pettibon Biomechanics Institute, those scientists helped to elevate our understanding of the spine to its current level.
In the Pettibon research program the principles of engineering that were first attributed to the ancient Egyptians in their design and construction of the Great Pyramids were found to be fundamental in the functioning of the human spine. In the spine we find a series of primary and secondary lateral curves that incorporate a system of lever arms, fulcrums, and pivot points that allow extraordinary freedom of motion while providing a high degree of resiliency, shock absorption, strength, and stability.
This explains how the seemingly impossible athletic feats we see in the performances of Olympic gymnasts like Laurie Hernandez and Simone Byles were made possible by the engineering characteristics of the spine discovered in Dr. Pettibon’s research. His research led to the specialty now known as Spinal Biomechanical Engineering.
In addition to being a mechanical marvel, the spine is the protector and conduit of the spinal cord and nerve roots as they transition from the central to the peripheral nervous system. At the same time, the spine is an active participant in the physiology and metabolism of the brain and spinal cord because of its participation in the primary sacral respiratory mechanism.
The primary sacral respiratory mechanism (PSRM) was eloquently described by Dr. Major DeJarnette, founder of the Sacro Occipital Technique (SOT) and the Sacro Occipital Research Society International (SORSI). In the primary sacral respiratory mechanism, the expansion and contraction of the rib cage in conjunction with the extension and flexion of the spine during the inspiration and expiration phases of respiration are not only the mechanisms of breathing, but provide the propulsion of cerebral spinal fluid in a wavelike motion up and down the spinal cord and around the brain and its system of ventricles.
The spinal motion of respiration and flow of cerebral spinal fluid (CSF) are examples of concurrent vital functions operating in interconnected and interdependent organs and systems. The CSF acts as a hydraulic shock absorber and lubricant between the brain and skull, the spine, spinal cord and nerve roots at the dural sheaths, lubricating their exit through the intervertebral foramina.
The CSF also fulfills an important role in the metabolism of the brain and spinal cord by providing the additional glucose they require over and above what is available in the arterial blood supply. The high glucose content of the CSF provides what could be thought of as an extra fuel injection system or turbo boost to supply the extra fuel that the central nervous system needs to function optimally.
Because the flow of CSF is dependent on the dynamic movement of the spine and respiration, any fixation of spinal motion, especially in flexion/extension, directly affects the efficiency of the primary sacral respiratory mechanism. Any loss of efficiency of the PSRM reduces the glucose available to the brain and spinal cord causing cerebral spinal glucopenia. This hypoglycemia of the central nervous system occurs despite the presence of normal blood glucose levels in the general circulation.
This is only one of several neurodynamic consequences of spinal dysfunction, which does not include the simplistic “bone out of place pressure on a nerve” explanation of the chiropractic lesion. Although the concept of a bone out of juxtaposition with the bone above, below, or both is passe, the spine does indeed misalign. The misalignment does not occur segmentally, but regionally in groups of vertebrae called spinal motor units.
The Pettibon Spinal Model
graphically depicts the normal, upright human spine as having six motor units as seen on the A to P and lateral views of a vectored spine.
The six spinal motor units are:
1. Skull and 4. T3-T7
Atlas 5. T8-L2
2. C2-C5 6. L3-S1
3. C6-T2
The misalignments of the spine consist of translations and rotations of the six spinal motor units in the x, y or z planes. Deviations of the spinal motor units from their normal aligned position are caused by one or a combination of causative factors.
“Injury during the birth process is a frequent cause and can predispose the person to future subluxations due to damage of the supportive ligaments of the cervical spine. Birth injury to the cervical spine has been implicated in what has been erroneously termed by the medical community as idiopathic scoliosis
Dennis Woggon DC, Scoliosis Expert, Founder of the CLEAR Institute
The common causes of the subluxation complex are either by an instantaneous, high velocity concussion of force, as in an automobile accident, bad fall or athletic injury, or by sustained force applied over time as occurs in occupational postural stress and repetitive motion injury. Additionally, excess body weight causes unbalanced forces that must be borne by the spine and can be counterbalanced only by compensatory muscle contraction, which compress the spinal weight-bearing surfaces and limit full spinal range of motion.
The neurological consequences of spinal misalignment most often begin with the reduction of the radius of the lateral curves of the cervical and lumbar spine. Geometrically, the ideal cervical and lumbar curves have a 60-degree arc in which the cord and radius are equal, forming an equilateral triangle.2
This degree of curve provides the most effective distribution of weight to resist the force of gravity to avoid buckling.3
There are multiple liabilities attached to the loss of the cervical and lumbar lordotic curves. The loss of these curves causes an increase of spinal cord and dural tension by as much as 24%.
Increased dural tension compresses the entire length of the spinal cord with as much as 30 to 40 pounds per square inch of pressure via a mechanism identical to the Chinese finger cuffs that tighten progressively as tension is applied.
Dr. Alf Breig, Nobel prize-winning neurosurgeon, described the increased spinal cord tension resulting from loss of cervical lordosis as “adverse tension.”
Increased dural tension and compression reduces CSF flow by restricting the subarachnoid space and by reducing the full spinal flexion and extension cycle.
Loss of the normal spinal curves causes a proportional loss of spinal shock absorption by shortening the length of the lever arms that the musculature of the spine needs for mechanical advantage and efficiency of movement.
Thoracic fixation, flattening of the normal thoracic kyphosis, and the deformation known as the Pottenger’s Saucer are the result of the loss of the cervical curve.
A spine with a full complement of curves is 26 times stronger than a perfectly straight or military spine, as described by Kapandji in The Spinal Engine, third edition. The relative strength of the spine is calculated by the number of intact curves squared plus one, which in a spine with all normal curves would be (52 + 1 = 26). In practical terms that means a person with a military spine has to exert much more energy to stand upright against the force of gravity than does a person with five normal spinal curves.4
Excessive contraction of the spinal musculature has the effect of reducing intervertebral motion while compressing the spine, especially at the pivotal or stress points located at the interspaces of C5-6, T7-8, and L2-3. These are also the locations of the thickest parts of the spinal cord and the narrowest parts of the neural canal.1
Compression of and constant impact on the crystalline mineral components of the bone causes the generation of piezo-electric and pyro-electric charges and streaming potentials from surrounding osseous structures. Vertebrae are normally electronically neutral. However, when stressed they will generate uneven electrical fields that can cause either impedance or excitation of nerve impulses transmitted through the spinal cord.5
This is why we predictably find the formation of spurs and lipping on the vertebrae in areas of maximal stress where points of compression cause the bone to produce a negative charge which draws the positively charged calcium ions to be deposited on the edges of the vertebral bodies and facets. This is the mechanism behind the formation and progression of osteoarthritis. This same electronic phenomenon occurs at stress points on the spine creating electrical impedance to the transmission of nerve impulses as they traverse these spinal levels.
When the spine is in its normally aligned and balanced position, it requires minimal muscular effort and energy to stand upright against the force of gravity.6
Dr. Roger Sperry (Nobel Prize Recipient for Brain Research) demonstrated that 90% of the brain’s energy output is used in relating the physical body to gravity. Only 10% has to do with thinking, metabolism, and healing. As a result, the brain will channel energy from thinking, metabolism, and immune function to deal with the challenges of abnormal postural relationships to gravity.
In a normally aligned spine the vertebrae enjoy electrical neutrality or a balanced surface electrical field. When the six spinal motor units depart from their properly aligned and balanced position, uneven forces and pressures are applied to the osseous structures, which cause the bone to take on uneven electrical charges. Research has shown that forces as light as 20mm of mercury pressure can produce electrical impedance reducing nerve flow and conductivity by as much as 50%. 7
H. Athenstaedt (1974, New York Academy of Sciences) discovered that the spinal cord and nerves are permanently di-polar. The negative pole is headward and the positive pole footward, causing nerve energy to flow from “above down and inside out.” When placed under uneven compression or tension bone will generate an unbalanced electrical field. This can cause either impedance or amplification of nerve impulses passing through the spinal cord and nerves. 1
This provides scientific validation of D.D. Palmer’s description of nerve interference as being “too much or too little nerve flow.”
Dysafferentation is yet another important consequence of spinal misalignment. It is stress related information transmitted to the motor cortex of the brain by the joint, tendon, ligament, and muscle mechanoceptors.
When processed by the brain, this stream of information initiates the adaptative and compensatory response to injury. It is experienced in the body as antalgic postures and persistent splinting spasms of the muscles. These guarding mechanisms are designed to stabilize and protect injured areas.
The ability of the brain to reprogram in response to the proprioceptive information it receives is known as neuroplasticity. Altered proprioception creates revised brain images of the injured areas. Fortunately, neuroplasticity allows restoration of normal motor cortex control patterns when the mechanoceptors are reset and normal afferentation returns.
Twenty-first century chiropractic provides us with the technology to move beyond repetitious manual adjusting as our only means of spinal correction. Advanced instrument adjusting techniques take chiropractic spinal correction to a new level of effectiveness by accessing and utilizing the postural control function and neuroplasticity of the brain to facilitate the restoration of normal spinal alignment and body balance. This constitutes a refinement in chiropractic care that uses more finesse than force.
The neurodynamic consequences of spinal misalignment and the vertebral subluxation complex provide the explanation for the broad scope of ill health, pain, and energy depletion that much of our population experiences. It is the genesis of disease, immune system suppression, imbalanced body chemistry, and ultimately, pathology. This should provide ample justification and incentive for the restoration and maintenance of a healthy aligned spine.
In reality, the vertebral subluxation complex literally short circuits the human power and communications grid causing a continuous drain on the energy resources that constitute our life force.
It is my conviction that every patient who honors me with their trust and confidence deserves the best care that I can provide through state of the art chiropractic care.
References
1. Petti bon, B., Introduction to Spinal Biomechanics, 1989.
2. Liddy, J.R., Modern Prestressed Concrete: Design Principles and Construction, 1978.
3. Kapandji, I.A., The Physiology of the Joints, 1974.
4. Kapandji, I.A., The Spinal Engine, Third Edition, 1978.
5. Basset, C.A.L., Becker, R.O., and Bachman, C.H., Bone Biodyncimics, 1964.
6. Sperry, R.W., Roger Sperry's brain research, Bulletin of the Theosophy Science Study Group 26(3-4), 27-28. Nerve Connections. Quart. Rev. Biol. 46, 198.
7. Sharpless, S.K, Proceedings of the 4th Biomechanics Conference on the Spine, University of Colorado, 1974.
Dr. William H. Koch, a 1967 Palmer graduate, just began his 52nd year as a chiropractic physician, writer and technique instructor. He has practiced successfully in the Hamptons of New York, The Bahamas, and Florida. Still in active practice, he currently splits his time between Abaco, Bahamas and Mount Dora, Florida.
Now, wanting to give back to the profession he loves, he offers courses on "The Koch Protocols for Integrated, Advanced, Chiropractic Techniques." Simple, Effective, No Nonsense and Hands-On.
Email Dr. Bill at outislanddc@ drwilliamhkoch.com or check out drwilliamhkoch.com.
 View Full Issue
View Full Issue