Helping Your Patients Get Back in the Game
June 1 2025 George RothHelping Your Patients Get Back in the Game
June 1 2025 George Roth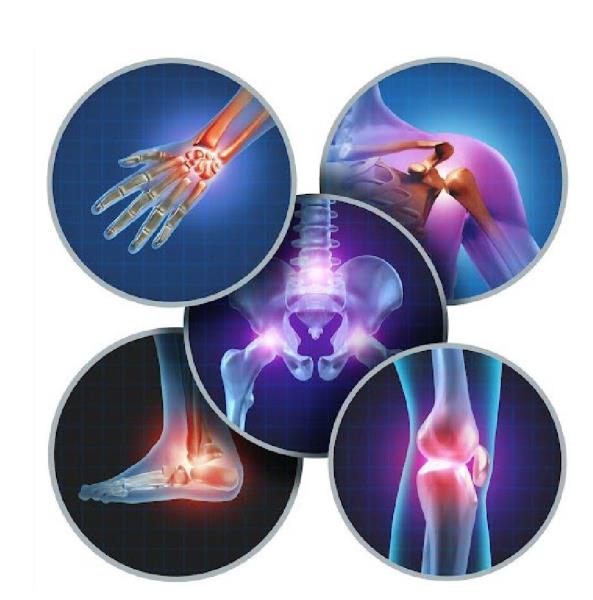
Many active people are forced to give up their favorite sports due to recurring joint pain, instability, or limited mobility—despite trying countless treatments. Dr. Roth shares insights from over four decades of clinical exploration, revealing a breakthrough understanding of joint instability and a gentle, science-based approach that’s helping patients worldwide return to active, pain-free lives.
Most active people eventually give up on their favorite sports for the same reasons. Whether it’s racquet sports, basketball, baseball, or hockey, they typically complain that either their knees “give out,” their low back “goes out,” or they are experiencing pain and limited movement in their hips, ankles, and shoulders.
They may have tried all kinds of treatments and strategies to stay in the game — chiropractic, physical therapy, exercise, lumbar supports, knee braces, taping, and the list goes on — but they eventually throw in the towel. It’s unfortunate since we know that maintaining an active lifestyle, including participating in sports, is a key element to support long-term physical and mental health.
Like most of you, I have often wondered why some patients seem to reinjure themselves repeatedly. They would get some temporary relief but still came back repeatedly with the same or similar issues, which I found very frustrating.
In this article, I would like to share some of the results of my ongoing exploration into the underlying mystery of how the body responds to injury at the deepest levels and the breakthrough discoveries I have made in over 40 years in practice. This culminated in the development of a gentle, science-based treatment system that has allowed practitioners from around the world to provide their patients with real solutions to many challenging conditions, helping them overcome pain and allowing them to enjoy a more active and abundant lifestyle.
If you have followed my work over the years, you may have read about the issue of joint instability and how undetected, deeper, underlying injuries may cause it. This is the condition I have referred to as the “articular stability reflex,” which I discovered by accident over 30 years ago while treating a young patient for low back pain.
Long story short, correcting the patient’s lumbosacral injury, also immediately restored the stability in his knee. He had been scheduled for ACL repair surgery, which was subsequently canceled when the surgeon confirmed complete resolution of the condition.
That case got me thinking. How had his knee regained stability? Did my treatment have anything to do with the improvement? A pattern began to slowly emerge, demonstrating a rather consistent association with injuries in other areas of the body that somehow seemed to be associated with knee instability.
Once these areas of focal tissue injury, which I refer to as “primary restrictions,” were resolved, unstable knees, shoulders, hips, ankles, and even the lumbar spine would become stable and stay that way. At the time, I had no way to explain the mechanism of improvement other than observing this rather startling clinical manifestation.
The difference in the joints that tend to become unstable (leading to accelerated degeneration and arthritis) is that certain muscles provide a form of dynamic stabilization. For example, recent studies have postulated that the popliteus is an important dynamic stabilizer of the knee. It is intricately attached to several internal structures of the knee, including the lateral meniscus, the posterior capsule of the knee, the PCL, and the MCL.12 3
I have also discovered that anterior instability of the knee is often accompanied by a reduced tone of the medial hamstrings (semimembranosus, semitendinosus) (Figure 1), which correlates with a positive anterior drawer test, as opposed to the often-erroneous assumption that it is caused by a tom or strained ACL. Additional muscular and fascial associations appear to mediate ankle stability (tibialis anterior). In the shoulder, a similar mechanism has been identified regarding the possible role of the supraspinatus as a stabilizer of the glenohumeral joint (Figure 2).4
 Figure 1: Dynamic Knee Stabilizers
Figure 1: Dynamic Knee Stabilizers
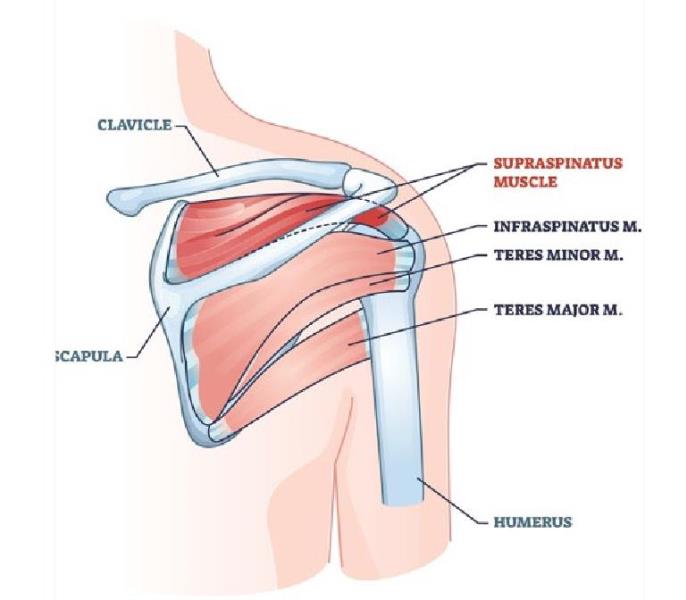 Figure 2: Shoulder stability provided by supraspinatus muscle.
Figure 2: Shoulder stability provided by supraspinatus muscle.
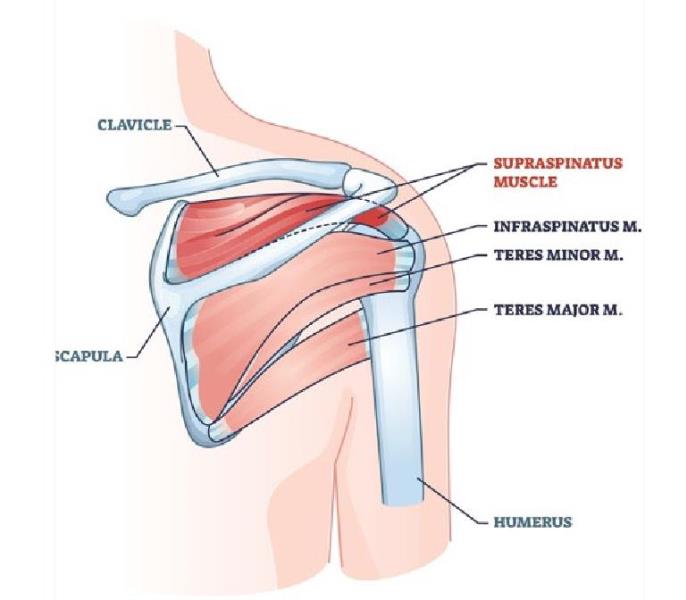 Figure 2: Shoulder stability provided by supraspinatus muscle.
Figure 2: Shoulder stability provided by supraspinatus muscle.
As I reviewed the areas containing the primary restrictions that seemed to be associated with joint instability, I noticed that they were invariably located in the cranium, spine, rib cage, or pelvis — the so-called core structures of the body. Treatment of these areas usually resulted in the restoration of stability in the involved peripheral joints almost instantly. The one exception was the lower lumbar spine, which is in the core region, and it proved to be a key to my understanding of this important mechanism.
“Once these areas of focal tissue injury were resolved, unstable knees, shoulders, hips, ankles, and even the lumbar spine would become stable and stay that way.”
I postulated that instability in the peripheral joints may protect the core structures (especially the spinal cord) from additional mechanical strain and potentially debilitating or even life-threatening damage. The knee, ankle, shoulder, and wrist joints are completely dependent on soft tissue for stabilization and could serve the role of “sacrificial joints” (Figure 3).
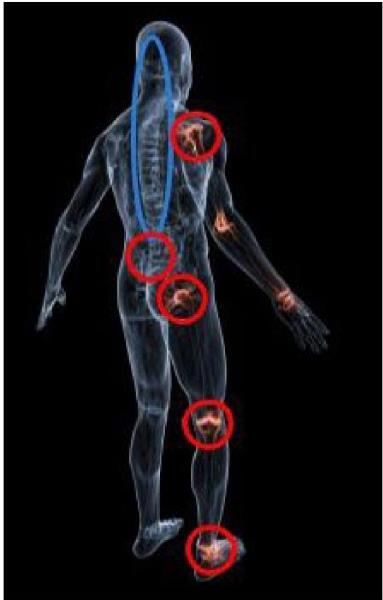 Figure 3: Sacrificial joints (red) and core structures (blue).
Figure 3: Sacrificial joints (red) and core structures (blue).
That term is adapted from the concept of sacrificial gears, which have been used with industrial machinery, such as printing presses, where specific gears constructed of less robust materials are situated at noncritical points in the device. These are deliberately designed to fail and disintegrate should the machinery become severely compromised, thus protecting more critical components.
What about the lower lumbar spine? The spinal cord is a key core structure that must be protected, but it typically ends at L2 or L3. The neurological structures of the lower lumbar spine (cauda equina), composed of separate, myelinated nerve tracts, are much less vulnerable to serious damage.
Lumbar stability appears to be related to the influence of multifidus and rotatores tone, as confirmed in recent studies5. Correcting primary restrictions in key core structures also tends to turn these muscles back on almost immediately, thus restoring stability and allowing for potential resolution of lumbar dysfunction. Turning Joint Stability Back On: Like Flipping a Switch
As I mentioned, treatment of primary restrictions in these core structures appears to immediately restore stability in these joints. What might account for this response? My current theory is that there may be a feedback mechanism mediated via spinal reflexes or mechanical-electro-chemical signals generated within the extracellular matrix (ECM).6-7-8 9
These systems may be able to monitor potentially threatening injuries and respond by triggering inhibitory or excitatory efferent neurons (spinal/neurological level). Whatever the mechanism may be, it appears to rapidly restore stability in many of the joints that get in the way of people enjoying the benefits of many sports activities.
Practitioners trained in Matrix Repatteming have helped many conditions associated with joint instability, resulting in significant clinical improvement. Further research is required to assess the effectiveness of this approach on the possible reversal or prevention of degenerative changes associated with these joints.
Dr. Roth is a graduate of the University of Toronto, Canadian Memorial Chiropractic College and the Ontario College of Naturopathic Medicine and has studied osteopathic medicine at Doctors’ Hospital North, Columbus, Ohio. He is the developer of Matrix Repatterning and is the Director of Education at the Matrix Institute in Toronto. His work is also featured in the Brain’s Way of Healing, by Dr. Norman Doidge, (Penguin, 2015). Visit matrixrepatterning.com or call 877-905-7684.
References
1. MacIntyre I. Anatomy and Function of the Popliteus Muscle. E-book; 2009.
2. Schinhan M, Bijak M, Unger E, Nau T. Electromyographic study of the popliteus muscle in the dynamic stabilization of the posterolateral comer structures of the knee. Am J Sports Med. 2011 Jan;39(l): 173-9. doi: 10.1177/0363546510377448. Epub 2010 Aug 31. PMID: 20807859.
3. Pasque C, Noyes FR, Gibbons M, Levy M, Grood E. The role of the popliteofibular ligament and the tendon of popliteus in providing stability in the human knee. J Bone Joint Surg Br. 2003 Mar;85(2):292-8. doi: 10.1302/0301-620x.85b2.12857. PMID: 12678372.
4. Van Linge, Mulder JD. Function of the supraspinatus muscle and its relation to the supraspinatus syndrome: an experimental study in man. J Bone Joint Surg Br. 1963 Nov;45(4):7504. PMID: 14074328.
5. Shahidi B. Hubbard JC, Gibbons MC, Ruoss S, Zlomislic V, Allen RT, Garfin SR, Ward SR. Lumbar multifidus muscle degenerates in individuals with chronic degenerative lumbar spine pathology. JOrthopRes. 2017 Dec;35(12):27002706. doi: 10.1002/jor.23597. Epub 2017 May 23. PMID: 28480978; PMCID: PMC5677570. "
6. Ingber DE. The architecture of life. Sci Am. 1998 Jan;278(l):48-57. doi: 10.1038/scientificamerican0198-48. PMID: 11536845.
7. MacGuintie LA. Streaming and piezoelectric potentials in connective tissues. In: Blank M (ed) Electromagnetic fields: biological interactions and mechanisms. Advances in Chemistry Series 250. American Chemical Society: Washington DC; 1995. doi: 10.1021/ba-1995-0250.ch008
8. Roth GB. The Matrix Repatterning Program for Pain Relief New Harbinger Publications: Oakland, CA; 2005.
9. Pischinger A. The Extracellular Matrix and Ground Regulation: Basis for a Holistic Biological Medicine. North Atlantic Books'. Berkley; 2007.
 View Full Issue
View Full Issue