Functional Leg Length Inequality in Performance
Dr. Brian Jensen
One of the most prevalent physical observations in chiropractic patients is the so-called “short leg.” This phenomenon has been rigorously investigated since the early days of chiropractic. Leg length inequality (LLI) can be classified as functional or structural and frequently involves a combination of both.
Understanding Structural Leg Length Inequality (SLLI)
Structural (anatomical) leg length inequality (SLLI) points to a condition where an actual difference in the length of the lower limb bones exists, particularly the femur, tibia, or fibula. This difference in bone length can occur because of various reasons, including congenital factors, growth abnormalities, trauma, or surgical procedures. SLLI is most accurately measured via a series of X-rays, wherein the lengths of the femur and tibia are quantified.
One efficient and practical method for gauging SLLI is by employing Allis’ or Galeazzi’s test. In this procedure, the patient lies supine on the table with the pelvis balanced in the transverse and frontal plane. The knees are then bent, and the medial malleoli are placed together so that the lengths of the femurs can be assessed from above. Tibial lengths can be determined by comparing the levels of the tibial plateaus.1
Another factor to consider when evaluating SLLI is the angle of the femoral neck, focusing on discerning any variation between the angles of the right and left femoral necks.
The Functional Leg Length Inequality (FLLI) Condition
Functional leg length inequality (FLLI) refers to a condition where the lengths of the lower extremities appear unequal during specific movements or positions despite similar anatomical lengths. This could result from factors such as muscle imbalances, joint restrictions, or biomechanical faults rather than a structural difference in the length of the bones.
To fully understand the contributing factors to LLI, the structural and functional components should be considered. The feet, being the primary point of contact with the ground, can be evaluated accurately only in their functional position of full weight-bearing. Measuring navicular drop or scanning the feet in a full weight-bearing position can give the information required to determine if the feet contribute to LLI.
Leg length inequality is observed in most patients, and its correlation with spinal dysfunction, gait biomechanical distortions, athletic performance, balance, and strength are well documented. While balancing out the LLI during an adjustment is regularly accomplished, the commonly unanswered question is, “What happens when the foot hits the ground?”
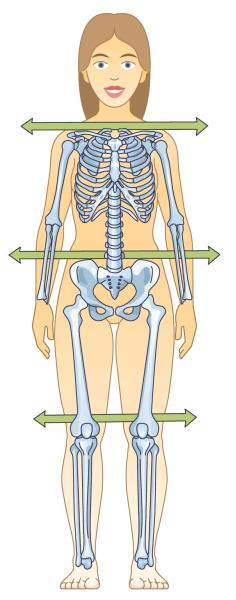 BALANCED
BALANCED
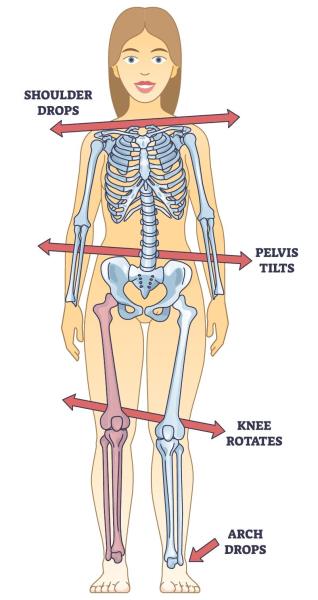 IMBALANCED
IMBALANCED
LLI Impact on Spinal Health and Biomechanics
Specht and De Boer reviewed the radiographs of 106 patients with leg length discrepancies (LLDs) greater than 3 mm.2 LLDs greater than 6 mm (53% of the cases) were associated with at least one abnormal spinal adaptation. Spinal adaptations included scoliosis, hypolordosis, and hyperlordosis. Similarly, Giles and Taylor studied the vertebral differences in 100 patients aged between 19 and 61 years old who had lower back pain and LLDs greater than 9 mm or within the range of 0 to 3 mm. They discovered a high prevalence of functional scoliosis with the curve’s convexity leaning toward the shorter leg among individuals comprising an LLD greater than 9 mm.
In addition, structural changes in vertebral morphology on the side of the shorter leg were observed. Such structural changes included increased L5 vertebral height and inferior end-plate asymmetry of the apical vertebra. Traction osteophytes were also observed in patients over 40 years old, suggestive of degenerative changes in the spine in response to long-standing functional scoliosis. Giles and Taylor thus concluded that superimposed functional scoliosis was likely to accelerate the rate of disc degeneration.3
Addressing LLI: Corrective Approaches
Determining how much lift is necessary to address LLI can be determined by measuring the femoral head height difference on that AP lumbopelvic X-ray and comparing it to the film with custom orthotics. The LLI disparity between the non-orthotic X-ray and the film with orthotics equates to the functional LLI. If a significant LLI persists, a lift can be utilized.
The right type of support can help. Custom flexible orthotics (in this case, called spinal pelvic stabilizers) obstruct excessive pronation and allow symmetric foot function. They have been demonstrated to resolve significant amounts of LLI. If there is a structural component related to the length of the femurs, tibias, or femoral necks, heel lifts can be added to address the anatomical component.
Consequences of Untreated LLI and Progress in Treatment Approaches
Failure to address LLI leaves the patient with a persistent structural and functional imbalance that affects gait, posture, balance, and fine motor control. For non-athletic patients, these deficiencies lead to chronic pain and degenerative changes. As for athletic patients, these irregularities lead to diminished athletic performance, inflammatory responses, and a heightened risk of injury.
Leg length inequality, a recognized contributor to pain and disability, has been documented for centuries. Early chiropractors recognized this and began studying the effect of chiropractic care on LLI. The invention of the spinal pelvic stabilizer by Dr. Monte Greenawalt in the early 1950s offered a solution to a significant and ubiquitous cause of functional leg length inequality and a strategy to correct it after the patient got off the table. Everything changes when the foot hits the ground. Today, we have the tools to intervene and manage the detrimental effects of leg length inequality.
References
1. Cooperstein R, Haneline M, Young M. Mathematical modeling of the so-called allis test: a field study in orthopedic confusion. Chiropr Osteopat. 2007 Jan 22;15:3. doi: 10.1186/1746-1340-15-3. PMID: 17241470; PMCID: PMC1796883.
2. Specht DL, De Boer KF. Anatomical leg length inequality, scoliosis and lordotic curve in unselected clinic patients. J Manipulative Physiol Ther. 1991 Jul-Aug;14(6):368-75. PMID: 1919374.
3. Applebaum A, Nessim A, Cho W. Overview and spinal implications of leg length discrepancy: narrative review. Clin Orthop Surg. 2021 Jun;13(2):127-134. doi: 10.4055/cios20224. Epub 2021 May 18. PMID: 34094002; PMCID: PMC8173231.
About the Author
Dr. Brian Jensen is a graduate of Palmer Chiropractic College and owner of Cave Spring Chiropractic in Roanoke, Virginia. He has been in practice for over 35 years. As a member of the Foot Levelers Speakers Bureau, he travels the country sharing his knowledge and insights. Watch continuing education seminars with Dr. Jensen and other Foot Levelers Speakers at footlevelers.com/continuing-education-seminars.
 View Full Issue
View Full Issue