How bone size may be affecting clinical outcomes
February 1 2024 George RothHow bone size may be affecting clinical outcomes
February 1 2024 George RothBone: Size Matters
PERSPECTIVE
How bone size may be affecting clinical outcomes
George Roth, DC, ND, CMRP
AS AN INTERN OVER 45 YEARS AGO, I noticed something mysterious. When I compared bilateral radiographic images of hips, knees, and shoulders, it appeared that the epiphyses on one side were noticeably larger than those on the other side. I mentioned this to the radiology department head, and he did not have an explanation. In addition, the larger side often displayed more arthritic changes, such as articular degeneration, sclerosis, and osteophyte formation.
At the time, I was also an instructor in the dissection lab, where I verified that asymmetry in bone size in these structures was fairly common. These differences were also noticeable in the articular processes, transverse processes, and bodies of vertebrae. These observations made me question several of my assumptions about what might be causing joint abnormalities. Over the years, I successfully developed strategies to address these bone changes. Eventually, evidence began to emerge supporting the concept of bone enlargement and its clinical implications
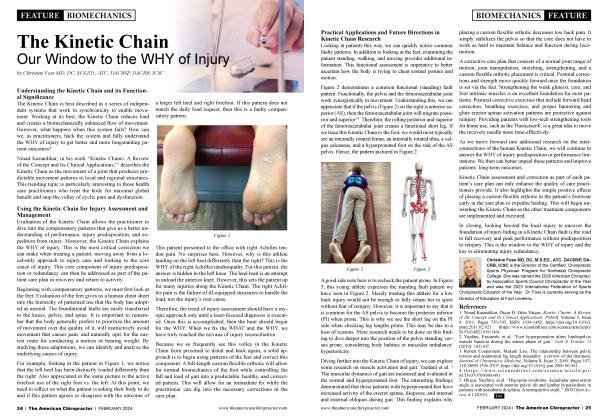
 Figure 1: Microscopic Evidence of Bone Expansion with Injury Paul Hansma Lab, University of California, Berkely, 2005.
Figure 1: Microscopic Evidence of Bone Expansion with Injury Paul Hansma Lab, University of California, Berkely, 2005.
Research Confirms Bone Enlargement with Injury and its Correlation with the Development of OA
Thirty years after my initial discoveries, research under the direction of physicist Dr. Paul Hansma at the University of California confirmed my observations1. Using the powerful Atomic Force Microscope (AFM), his team verified the structural effects of injury within bone at the cellular and molecular levels. It revealed that bone changes shape and gets bigger with injury (Figure 1).
Evidence from a study conducted by a team from the Department of Epidemiology and Preventive Medicine, Monash University, also found a correlation between relative bone enlargement and the development of osteoarthritis:
“Bone size, both adjacent to and distant to affected joints, has been shown to correlate with the severity of osteoarthritis. A recent study which examined the relation between tibia1 plateau area and early changes of radiographic knee osteoarthritis found a positive association between grade I osteophytosis and tibial plateau area. ”2
These findings made me wonder why these bone changes were never discussed in our chiropractic education and how they might be implicated in our interpretation of vertebral subluxations.
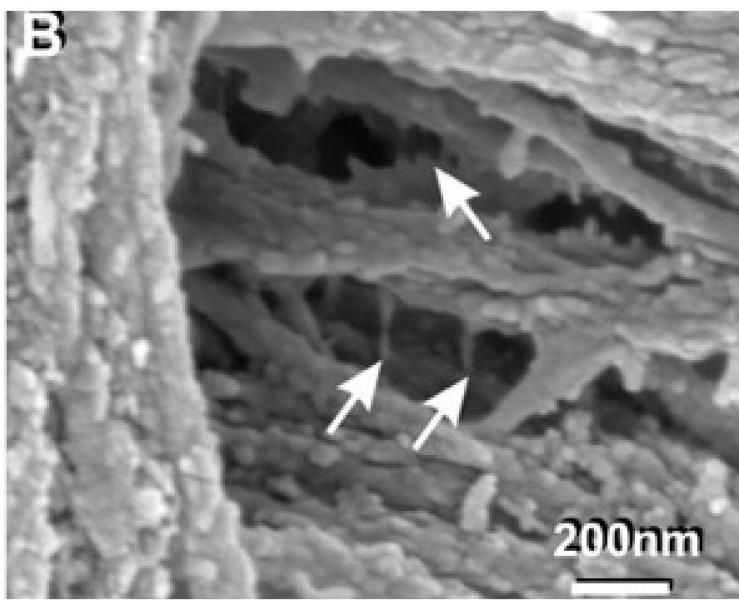 Figure 1: Microscopic Evidence of Bone Expansion with Injury Paul Hansma Lab, University of California, Berkely, 2005.
Figure 1: Microscopic Evidence of Bone Expansion with Injury Paul Hansma Lab, University of California, Berkely, 2005.
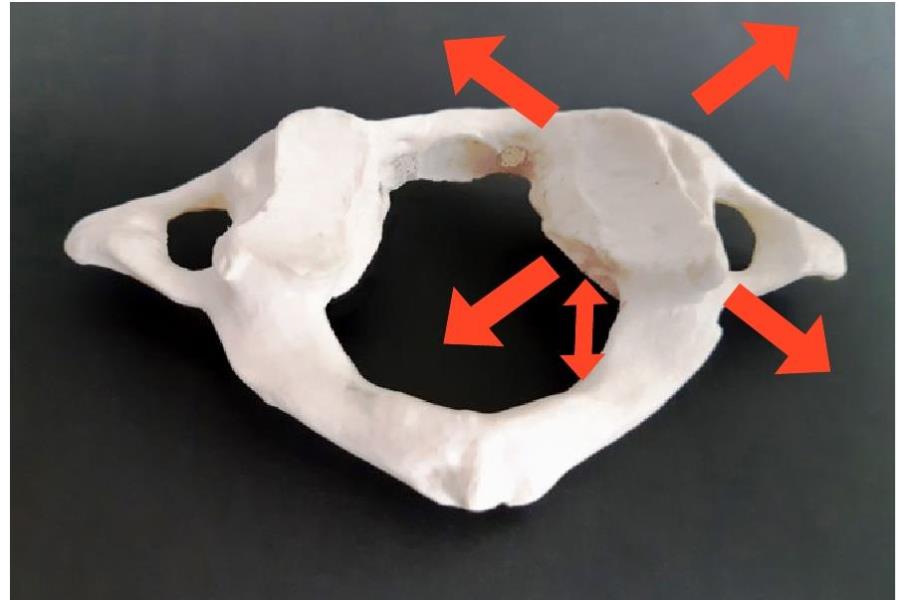 Figure 2: C1, cast from a skeletal specimen. Note the enlargement of one of the articular processes and the spinal canal, which measure 2 mm. larger in every dimension.
Figure 2: C1, cast from a skeletal specimen. Note the enlargement of one of the articular processes and the spinal canal, which measure 2 mm. larger in every dimension.
Is Vertebral Subluxation a Case of Mistaken Identity?
Actual measurement of vertebral specimens at multiple levels throughout the spine indicate differences in the size of anatomical structures on one side versus the other (e.g., width, depth, and height of the vertebral body, articular processes, and lamina or transverse processes), verifying many of the same osseous changes I observed as a student. Figure 2 illustrates these differences in the size of the articular processes of C1. These enlarged structures might be easily mistaken for a relative rotation or translation of the vertebral segment. Additional evidence of osseous asymmetry can be found throughout the spine (Figures 3, 4).
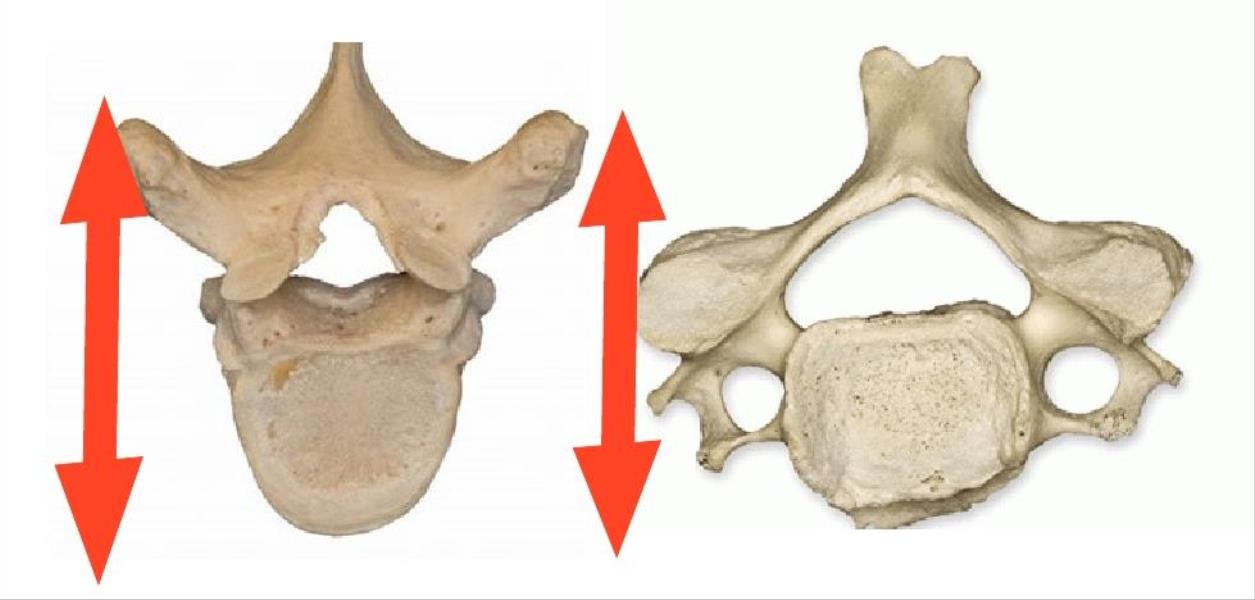 Figures 3, 4: Cervical and thoracic vertebrae. Note enlargement of the vertebral body and articular process on one side compared with the other.
Figures 3, 4: Cervical and thoracic vertebrae. Note enlargement of the vertebral body and articular process on one side compared with the other.
Case Study:
Steve* is a teenage hockey player who experienced significant pain in his left knee for over two years. After a series of six specialized treatments3 over two months, there was a significant reduction in the size of his left knee (approximately 5 mm.) as recorded by orthopedic specialists monitoring his condition (Figures 5, 6). He subsequently returned to hockey and resumed all of his nonnal activities. His parents remarked how delighted they were as they could once again “hear the sound of Steve running up the stairs,” instead of hobbling slowly and painfully as he had for the previous two years.
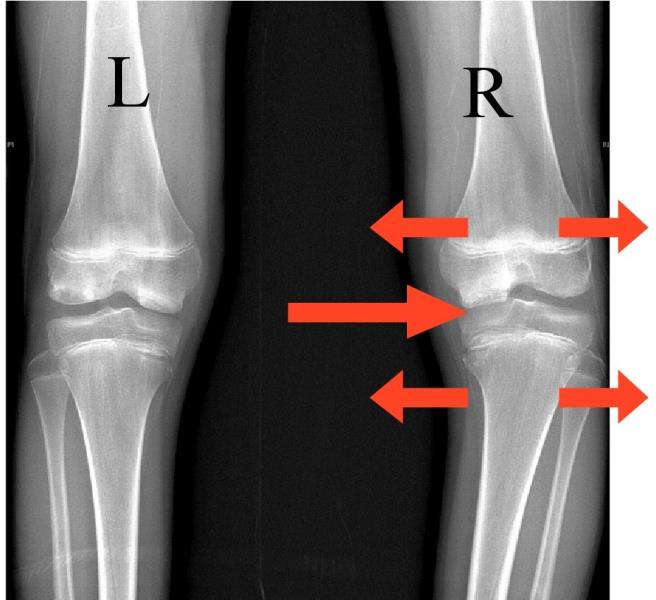 Figure 5: Pre-treatment
Figure 5: Pre-treatment
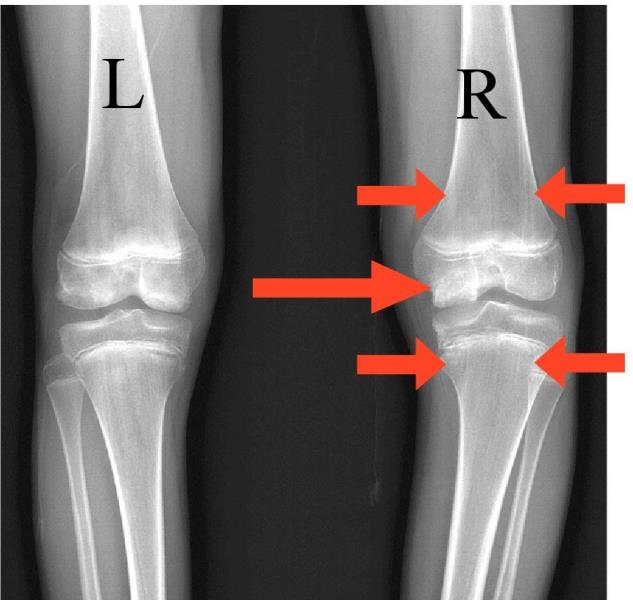 Figure 6: Post-treatment
Figure 6: Post-treatment
Note: Left Knee (pre and post treatment): 1. Femoral and tibial epiphyseal size reduced by approximately 5 mm. 2. Medial joint space improved..
Summary
The implications of this new understanding of the effect of injury on bone structure could hold the key to our success in relieving a multitude of painful and limiting conditions. In developing a new approach to treating these bone changes, I considered the scientific discoveries regarding how the body is constructed and how it responds to injury at the cellular level4'7. I recognized that injuries often resulted in structural changes within the densest structures of the body (the skeletal frame and the deep fascia associated with the fluid-filled organs). Symptoms such as strain, pain, and biomechanical dysfunction arising from the surrounding soft tissues (e.g., muscles, ligaments, and fascia) often appear to result from the mechanical stresses imposed on them by these changes. This gentle and non-invasive treatment has demonstrated measurable and objective results, such as radiographic, laboratory, and neurological improvement verified by independent radiologists, researchers, and clinicians8.
It is now proven that bone and other deep fascial structures are structurally altered by injury. As clinicians, we must take this scientific fact into account. It is my experience, and that of practitioners around the world using these methods, that resolving these deep, underlying aspects of injury can provide us with the opportunity to relieve suffering, restore optimal function, and achieve a higher level of practice satisfaction and success.
Dr. George Roth is a graduate of the University of Toronto, Canadian Memorial Chiropractic College, and the Ontario College of Naturopathic Medicine and has studied osteopathic medicine at Doctors’ Hospital North, Columbus, Ohio. He is the developer of Matrix Repatterning and Director of Education at the Matrix Institute in Toronto. Dr. Roth has presented seminars at numerous hospital and university-based symposia throughout North America. He is the co-author, along with Kerry D’Ambrogio PT, of Positional Release Therapy (Elsevier, 1997) and the author of The Matrix Repatterning Program for Pain Relief (New Harbinger, 2005). His work is also featured in the Brain’s Way of Healing by Dr. Norman Doidge (Penguin, 2016).
References:
1. Fantner GE, Hassenkam T, Kindt JH, Weaver JC, Birkedal H, Pechenik L, Cutroni JA, Cidade GA, Stucky GD, Morse DE, Hansma PK , Sacrificial bonds and hidden length dissipate energy as mineralized fibrils separate during bone fracture, Nat Mater. 2005 Aug;4(8):612-6. Epub 2005 Jul 17.
2. Wluka AE, Wang Y, Davis SR, et al, Tibial plateau size is related to grade of joint space narrowing and osteophytes in healthy women and in women with osteoarthritis, Annals of the Rheumatic Diseases 2005; 64:1033-1037.
3. Roth GB, The Matrix Repatteming Program for Pain Relief, New Harbinger Publications, Oakland, CA, 2005.
4. IngberDE, The Architecture of Life, Scientific American, Vol. 1, 1998.
5. Pischinger A, The Extracellular Matrix and Ground Regulation, Basis for a Holistic Biological Medicine, North Atlantic Books, Berkley, 2007.
6. Chakkalakal DA, Mechanoelectric transduction in bone. J Mater Res. 1989;4: 1034-1046.
7. MacGuintie LA, Streaming and piezoelectric potentials in connective tissues, In: Blank M (ed) Electromagnetic fields: biological interactions and mechanisms. Advances in Chemistry Series 250. American Chemical Society, Washington DC, ch. 8, pp 125-142, 1995.
8. Doidge, N., The Brain’s Way of Healing, Penguin Books, New York, 2016.
 View Full Issue
View Full Issue