Disc Nomenclature
CLINICAL EXCELLENCE
The Importance of Getting it Right
Mark Studin
DC, FASBE(C), DAAPM, DAAMLP
For chiropractic to compete in the spinal marketplace, we must be considered peers with our medical counterparts in spine care. Also, the legal community will not consider chiropractors a valuable solution in the courts without them being an expert. The most “basic” element of collaboration of a peer and being an expert is terminology. If we, as a profession, communicate as “laypersons” on medical terminology, we will have earned the reputation as technicians versus doctors and bypassed for collaboration or expert opinions. In part, that is why we are stuck in the cycle of 7% to 10% utilization that has plagued our profession for decades.
Our profession has worked tirelessly to ensure that we get recognition in the radiological community to be considered a peer. The American Chiropractic College of Radiology (ACCR) and American Chiropractic Board of Radiology are at the highest level for those who want to practice as a reading radiologist. There is a qualification in MRI interpretation review for practitioners who want to ensure the interpretation from the radiologist is accurate, recognized by chiropractic academia. The fellowship in primary spine care is certified by medical and chiropractic academia, with a strong focus on MRI interpretation to further ensure the interpretations are correct. If you choose to participate, it is critical that you, as a practitioner, use “contemporary evidence-based nomenclature” because the lack thereof will not only hurt your reputation but also injure the chiropractic profession.
Using terms such as “slipped or prolapsed disc” and other colloquial or noncontemporary evidence-based nomenclature in collaborative or expert relationships are examples of how to destroy relationships. When considering terminology, the research article by Fardon et al. titled “Lumbar Disc Nomenclature: Version 2.0: Recommendations of the Combined Task Forces of the North American Spine Society, the American Society of Spine Radiology, and the American Society of Neuroradiology” has guided contemporary documentation used in medical and chiropractic academia. This paper was also cited by 454 other indexed peer-reviewed articles, making it a well-recognized authority in the scientific community.
Fardon et al. reported:
The paper “Nomenclature and Classification of Lumbar Disc Pathology, Recommendations of the Combined Task Forces of the North American Spine Society, the American Society of Spine Radiology, and the American Society of Neuroradiology,” was published in 2001 in Spine (Lippincott, Williams & Wilkins). It was authored by David Fardon, MD, and Pierre Milette, MD, and formally endorsed by the American Society of Spine Radiology (ASSR), American Society of Neuroradiology (ASNR), and North American Spine Society (NASS). Its purpose was to promote greater clarity and consistency of usage of spinal terminology, and it has served this purpose well for over a decade. Since 2001, there has been sufficient evolution in our understanding of the lumbar disc to suggest the need for revision and updating of the original document. The revised document is presented here, and it represents the consensus recommendations of contemporary combined task forces of the AS SR, ASNR, and NASS. This article reflects changes consistent with current concepts in radiologic and clinical care. (p. 2525)
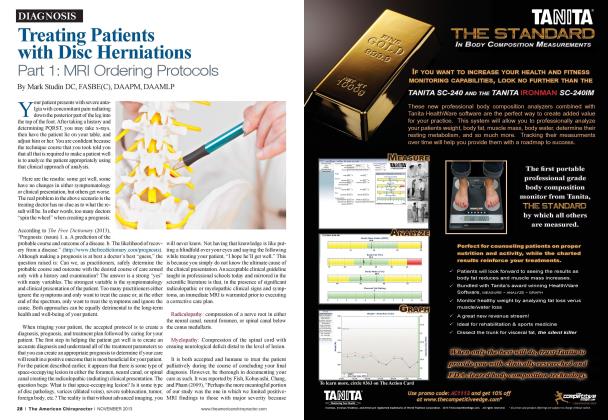
Terminology, as reported by Fardon et al. (2014): Herniation is broadly defined as a localized or focal displacement of disc material beyond the limits of the intervertebral disc space. The disc material may be the nucleus, cartilage, fragmented apophyseal bone, annular tissue, or any combination thereof. The disc space is defined as craniad and caudad by the vertebral body endplates and, peripherally, by the outer edges of the vertebral ring apophyses, exclusive of osteophytes. Herniated discs may be classified as protrusion or extrusion based on the shape of the displaced material.
Protrusion is present if the greatest distance between the edges of the disc material presenting outside the disc space is less than the distance between the edges of the base of that disc material extending outside the disc space. The base is defined as the width of disc material at the outer margin of the disc space of origin, where disc material displaced beyond the disc space is continuous with the disc material within the disc space.
MRI spine interpretation is one arena that will help catapult the chiropractic profession as primary spine care providers or the first option for spine management.
Extrusion is present when, in at least one plane, any one distance between the edges of the disc material beyond the disc space is greater than the distance between the edges of the base of the disc material beyond the disc space or when no continuity exists between the disc material beyond the disc space and that within the disc space. The latter form of extrusion is best specified or subclassified as sequestration if the displaced disc material has completely lost continuity with the parent disc. The term “migration” may be used to signify displacement of disc material away from the site of extrusion. Herniated discs in the craniocaudal (vertical) direction through a gap in the vertebral body endplate are referred to as “intravertebral herniations” (SchmorTs nodes).
Bulging disc:
1. A disc in which the contour of the outer annulus extends, or appears to extend, in the horizontal (axial) plane beyond the edges of the disc space, usually greater than 25% (90 degrees) of the circumference of the disc and usually less than 3 mm beyond the edges of the vertebral body apophysis.
2. (Nonstandard) A disc in which the outer margin extends over a broad base beyond the edges of the disc space.
3. (Nonstandard) Mild, diffuse, smooth displacement of disc.
4.Nonstandard) Any disc displacement at the discal level.
Note: Bulging is an observation of the contour of the outer disc and is not a specific diagnosis.
Those definitions give a basic understanding of disc pathology to ensure an accurate conversation with a collaborating physician. Still, they fail to make any doctor an expert without formal training (see previous suggestions). MRI spine interpretation is one arena that will help catapult the chiropractic profession as primary spine care providers or the first option for spine management. This is where we can start to break that 7% to 10% utilization cycle.
Dr. Mark Studin is the founder of the Academy of Chiropractic and the Doctors PI Program. He teaches chiropractic and medical at various levels and creates strategic business strategies for chiropractors, medical doctors, hospitals, and lawyers nationally. Reach Dr. Studin at 631-786-4253 or [email protected].
Reference:
1. Fardon, David F., et al. “Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. ” The Spine Journal 14.11 (2014): 2525-2545.
2. Google Scholar (2021) retrievedfrom: https: scholar.google.com scholar ?hl=en&as sdt=0 %2 C33 &q=fardon +lumbar+disc+nomenclature & b tnG=
 View Full Issue
View Full Issue