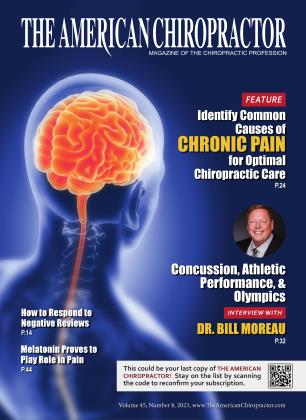
Dr. William Moreau, DC, DACBSP, FACSM, is an evidence-guided doctor of chiropractic who specializes in sports medicine. He practiced in Iowa for 30 years and then worked for 10 years leading sports medicine for the United States Olympic and Paralympic Committee. In 2017, the USOPC promoted him to the position of USOC vice president of sports medicine. In this position, he oversaw USOC sports medicine-related activities, including the delivery of health care at four Olympic Games and three USOC Clinics. He led the USOC National Medical Network and formulated medical standards of care for the USOC.
Moreau served as Team USA’s medical director at the London 2012 Olympic Games and the Sochi 2014 Olympic Winter Games. He became the only doctor of chiropractic to serve as chief medical officer at an Olympic Games for both the 2016 Summer Rio Olympic Games and the 2018 Winter Olympic Games in South Korea. As chief medical officer, he directed the health care for Team USA athletes.
The prevention of injury in athletics is an important component of athlete health and team success. Dr. Moreau founded the United States Coalition for the Prevention of Illness and Injury in Sport. This coalition is one of a limited number of the International Olympic Committee’s international centers of research excellence.
Dr. Moreau has more than 35 years of clinical expertise in sports medicine. He is dedicated to advancing patient-centered, evidence-guided clinical care pathways delivered through integrated multidisciplinary healthcare teams.
Dr. Moreau has delivered over 500 invited lectures and has been featured in Bloomberg Businessweek, USA Today, and TIME and on ESPN, NPR, NBC, and CBS Evening News.
Moreau is an avid conservationist. He lives with Karen Moreau in Vancouver, Washington.
Not pictured: Anna Gorbachuk, Melania Muller, Renata Retter, Steven Jerome, and Dr. Jasmine Piper.
TAC: What got you interested in treating athletes?
WM: While practicing in private practice decades ago in Iowa, it became clear to me that athletes and their parents were looking for a conservative care provider to help them with athletic injuries. I soon learned that sports medicine as a specialty is broad and deep. I knew that additional education was needed for me to provide the best care I could for my patients. This continuing journey to learn and earn certificates of additional qualifications with a sports medicine emphasis is something I enjoyed, and the quest to be better really provided a focus to my continued professional training over the past decades. An already busy practice became much busier!
Instead of trying a seminar here and there on different topics, the framework of sports medicine provided a focused tract of learning and a clear pathway to continued personal development. As my reputation in sports medicine grew, more opportunities became available to provide sports medicine care in the clinic setting and on the field of play at the high school and junior college level. All of these experiences helped me develop the skill set to work at the Olympic level. The Socrates maxim is true, “The more I learn, the more I leam how little I know.” It is great to start every day with the opportunity to improve and become a better doctor.
TAC: How has sports medicine changed over the years?
WM: When I started in sports many years ago, tradition was the way to provide care. Early in my career, difficult or unusual cases were solved by which books you had on your bookshelf and who you could call for help. Today, there is immediate access to tens of thousands of current journal articles on any topic that are just a click away. Traditional sports medicine textbooks are becoming obsolete because they are out of date as soon as they are published.
Another change is the now common inclusion of the doctor of chiropractic on the sports medicine team. It is common that a team of providers care for individual athlete(s) and sporting teams. For example, the average U.S. Olympic hopeful had 10 different healthcare providers looking after them at any one time. The concept of teamwork is at the forefront of today’s sports medicine care. The doctor of chiropractic’s role on the sports medicine team is defined, m part, by the other care providers on the team and the skill sets and experience of the individual.
TAC: How has the use of chiropractic on athletes evolved?
WM: This is a great question! At the start of my career, people were surprised to learn that a DC served as a team doctor. There were comparatively few DCs recognized by sporting organizations, and there were many skeptics that a DC could serve in any capacity, much less lead sports medicine health care. They were clearly wrong!
In the early days, the USOC credentialed few doctors of chiropractic with Team USA games credentials; there was one at the summer games and none for the winter games. Now there are dozens of DCs officially credentialed to provide service at Olympic and Paralympic Games. The USOPC employs DCs as full-time clinicians where they work along with all different types of healthcare providers. There are many DCs officially recognized and associated with high-level college athletic teams and throughout professional sport. My viewpoint is this explosion of opportunity is driven by the athletes who demand and drive the inclusion of DCs as a part of the sports medicine team.
TAC: Can you talk about the evolution of the data on concussion?
WM: For more than three decades, sports-related concussion has been an area of special interest for me. In the “not-so-distant” past, concussion evaluations were fairly crude, and care was simply watchful waiting. The tide of concussion care took a big turnaround in 2015 when respected organizations proclaimed there were pathways to care and improve concussion outcomes. Interestingly, there is no broadly accepted evidence that any medication can resolve a patient’s concussion. In 2015 and again in 2019, the non-DC American Medical Society for Sports Medicine’s position statements on concussion in sport stated, “Athletes with migraine/headache should be evaluated for underlying headache disorders, cervical dysfunction causing headache, and other possible contributors, and treated appropriately with non-pharmacological and pharmacological treatments.” It is fascinating that they advocate for what chiropractors can do, while our own profession (other than the American Board of Chiropractic Sports Physicians) has not clearly arrived at the same conclusion that the doctor of chiropractic may play an important role in the care of concussed individuals.
In the early days, adjustments to the cervical spine of acutely concussed individuals were generally considered contraindicated; now in certain cases chiropractic adjustments are indicated. My perspective is the chiropractic profession is losing cultural authority regarding concussion and manual procedures. Interested doctors of chiropractic need to get involved. Soft tissue care, gentle spinal adjustments, active care, ocular retraining, vestibular training, and many more skill sets help the DC provide the quality care the patient with concussion needs.
In adults who sustain a concussion, it is estimated that 70% -90% will recover without any intervention other than avoiding a second concussion. The population I am focused on is the 10% that do not recover. When injured individuals have concussive symptoms for longer than two months, the diagnosis changes to post-concussion syndrome. This is the new frontier of evaluation and management of these head-injured patients. At the University of Western States with Dr. Brimhall’s strong support, I direct a concussion clinic for individuals with post-concussion problems often exhibited as dysautonomia and postural orthostatic tachycardia syndrome (POTS). This ongoing work is the most important and personally significant work of my professional career.
TAC: What are some tests chiropractors can use to identify concussions?
WM: The first step to identifying a concussion is through a careful and accurate assessment. It is imperative to avoid the misdiagnosis of a more serious head injury. The skills of obtaining a history, obtaining vital signs, performing a thorough neurological examination (including a cranial nerve examination), using the concussion symptom checklist from the Standardized Concussion Assessment Tool (SCAT), and traditional cervical spine orthopedic testing is the minimum starting point. Additional tests should be learned and also used. Some useful ways to identify cervicogenic concussive concerns include the Joint Position Error Test, balance testing (modified BESS test), Smooth Pursuit Neck Torsion Test, Trail Making tests, Head Neck Differentiation Test, and King Devick testing.
TAC: Are these easy to learn?
WM: Any healthcare provider can learn these examination skills if they are interested in doing so. Like so many other areas of practice, careful research, preparation, and practice leads to clinical competency. None of these tests are difficult to perform. The interpretation of the test results is where difficulty comes into play.
TAC: How do you see guidelines around head trauma evolving?
WM: We are only starting to unravel the neuropathology of concussion. When we consider that four of the 12 cranial nerves relate to vision, it makes sense that, to have proper vision, this task produces a high CNS workload. Visual examinations can also provide objective evidence of concussion when nystagmus is identified. The visual examination is an area that needs to be explored further. We see this in the SCAT6 guideline that were just released. The SCAT6 increases the importance of the eye extennination as well as other important changes.
Additionally, with post-concussive patients, we are becoming much more aware of the assessments and diagnosis of autonomic nervous system dysfunction. I believe that the detection and management of dysautonomia in post-concussion patients will be the key to helping millions of head-injured people. We should prepare our skill sets to manage dysautonomia as this will become commonplace over the next few years.
TAC: Is the issue of concussion treated the same between males and females?
WM: Gender does play a role in concussion, but we do not really know why. Dr. Tracey Covassin from Michigan State University is one of the researchers I follow regarding gender and concussion. She identified that women basketball players have a 300% increased incidence of concussion in comparison to males. Covassin’s research suggests the incidence and recovery from sport-related concussion varies between male and female athletes, with women having a higher risk of sustaining a concussion and taking a longer tune to recover than men. The reason this occurs has not been definitively identified. We do know that menstrual cycle-related changes are not the cause. One possible reason is the body mass and size of the athlete may allow for a better distribution of concussive forces.
TAC: How is this different in kids or adults?
WM: Children clearly do not recover from concussion at the same pace as adults. Previously, I mentioned most of adults with concussion should resolve within two weeks. For the child and adolescent populations, the average time to recover is closer to four weeks. These young people may experience recovery more than three times longer if they fail to be seen by a concussion-trained healthcare provider within the early phases of their injury.
TAC: What do you see as being the greatest opportunity in sports medicine going forward?
WM: The opportunities for doctors of chiropractic to become involved in sports will continue to increase. It is important that the individual DC carefully evaluates the specific sports setting and identifies what their individual role will be on the sports medicine team. Generally speaking, the smaller the sports medicine team, the larger the opportunity to participate. Each opportunity, large or small, will provide both challenges and rewards. The individual needs to ensure they are a good fit before engaging as a part of the team. In the clinical setting, sports chiropractic has been on a growth trajectory for years. I see no reason this will not continue, and hope that the opportunity for the profession to serve grows exponentially.
TAC: Who are some of your favorite providers in the chiropractic profession?
WM: A special thanks should be offered to the many pioneers of sports chiropractic who paved the way for all of us to follow. Their then cutting-edge work directly led to an easier path for those of us who followed. There are so many pioneers in sports chiropractic that I will not attempt to name them for fear of leaving out an important chiropractic leader! My perspective is the best chiropractic leadership in sports medicine is yet to come. Today’s doctors of chiropractic are better trained and keen to be the best they can be; cheers to them!
TAC: Any final words for our readers? WM: I am thankful for all the profession has provided to me. The decision to become a doctor of chiropractic literally opened the world of learning and caring for me. I believe it is both a privilege and an obligation to hone our skills on a daily basis to best serve the people who present to us for care. Life is meant to be an adventure; embrace the adventure and explore who you can become.IfiSSI
For the ful1 interview with Dr Moreau and other TAC Tic Talks scan the QR or visit: Tic-talk.net
 View Full Issue
View Full Issue