Looking at the biomechanics of every patient with digital foot scans and digital x-rays.
May 2 2020 Tim MaggsLooking at the biomechanics of every patient with digital foot scans and digital x-rays.
May 2 2020 Tim MaggsI examine and treat a lot of middle and high school athletes. 3 years ago I had a very learning experience with one particular athlete. Josh was a 10th grade soccer player who went through our biomechanical exam to figure out why he had low back pain. Part of our exam consists of a digital laser foot scan, and we determined Josh needed custom orthotics. We also did our standard 2 view lumbosacral digital x-rays standing and barefooted. One critical measurement we look at is femoral head height difference (fhhd). Digital x-ray allows exact measurements, so this has now become part of every patient’s report of findings. Simply put, the goal for the femoral heads is level. Josh’s fhhd was 4.3mm (Fig. 1) In one week, Josh’s orthotics arrived and we showed him how to introduce them into his shoes and life.
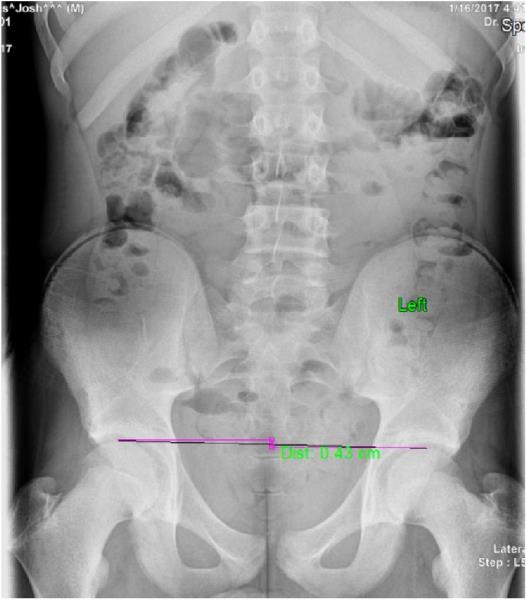 Fig. 1: Huckans apls 1 (4.3mm)
Fig. 1: Huckans apls 1 (4.3mm)
I continued to treat Josh at school as I went there once a week to treat many students. Within a couple weeks, Josh started complaining of a left apophysitis. I assumed it was a mild strain from soccer and applied laser therapy and kinesiotaped it along with my adjustment. Over the next 3 months, Josh continued complaining and his complaints grew louder. I told him to make an appointment in my office so I could examine him, and if necessary, rex-ray him. By the time his mother brought him in, it was so inflamed and painful he couldn’t play soccer. I started with a new A-P L-S x-ray with his orthotics on. With orthotics on, his fhhd was now 6.0mm. (Fig. 2) Further investigation showed a stress fracture at the site of pain. We then put a 5mm lift on the orthotic of the low femoral head, continued laser treatments (Fig. 3), and Josh healed very quickly.
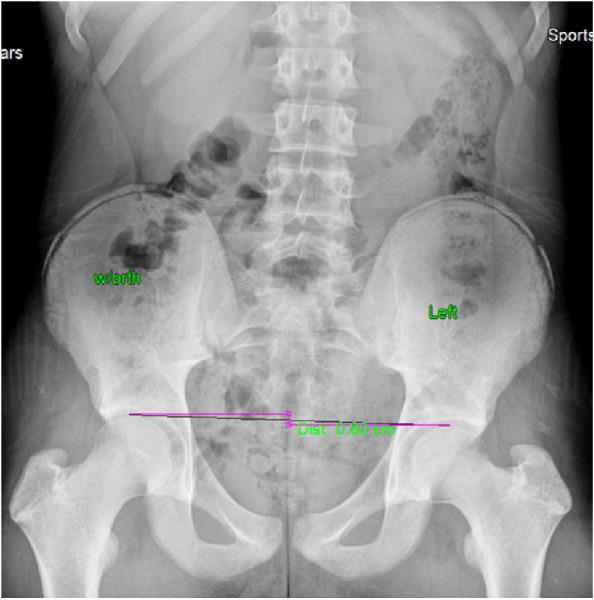 Fig. 2: Huckans apls 2 (6.0mm)
Fig. 2: Huckans apls 2 (6.0mm)
Although I’d never suspected that fhhd could increase with the use of orthotics, multiple times I had questioned the very possibility that the inclusion of custom orthotics created new problems but didn’t know why. If Josh’s fhhd was worse after orthotics were put in his shoes, how many other patients had this happened with? I now knew I needed to create new protocols. Was Josh the one in a million, or could there be a greater percentage whose fhhd worsened with orthotics? I decided I would continue my digital laser foot scan, I would continue ordering orthotics when there was any collapse of arches on the scan, but when the orthotics came in, I would put them in the patient’s shoes and re-take the A-P L-S x-ray with the shoes on to see what happens to their fhhd. Over the next 2 A years, I documented the findings from 308 patients.
When the loading of a tissue exceeds the capacity of that tissue, compensatory physiological changes occur.
For the past 15 years, I’ve become a student of the effects of abnormal loading. Our musculoskeletal industry has remained ignorant to the importance of loading and abnormal loading in the human body. The effort to reactively treat pain as the only goal, whether it be with a pill or a chiropractic adjustment, is a clear admission of short-sightedness. Chiropractic had always been about treating the cause of the pain, so I don’t know when some members of our profession switched up and partnered with the medical model of care approach that only concerns itself with symptoms.
I work with so many middle and high school athletes, and I teach them and their families that youth hides a lot of sins. The biomechanical faults that are identifiable in this age group are usually asymptomatic because the tissue has not yet been abused. But, with the proper tests, we can identify the abnormal biomechanical faults starting at the age of 12, and we all know abnormal loading is of great concern, not just the symptoms. With abnormal loading, the body will eagerly begin to adapt accordingly. This adaptation includes the negative physiological changes that lead to injuries. Calcium build-up will start, muscles will become more constricted, bursas will become inflamed, tendons will tighten and ultimately become inflamed and discs will begin to dessicate, degenerate, bulge and herniate. It’s all a matter of time. Some say “the body will adapt to the imbalances”. I agree, but they call that disease and degeneration. It’s the same process the body goes through if your blood chemistries are off. The body will adapt, but a disease process has begun.
Over the past 25 years, I have performed literally thousands of biomechanical exams, which include digital foot scans and standing cervical and lumbo-sacral x-rays. Every patient demonstrated biomechanical faults leading to the conclusion—Everyone is Crooked Man (Fig. 4). When you look at Crooked Man, you will recognize imbalances begin in the feet. If you don’t address the feet, you’re reducing the ultimate potential improvement of any patient’s biomechanical success.
So, in my quest to figure out what was going on with those patients whose fhhd increased with orthotics, I knew I couldn’t abandon the use of custom orthotics, but rather learn what more had to be done to reduce fhhd on every patient. I knew abnormal loading is a cumulative issue, so the importance of reducing abnormal loading and creating symmetry and balance remained Goal #1.
It’s also important to properly interpret the digital foot scan (Fig. 5). If the patient’s scan doesn’t exactly mirror the optimal scan, custom orthotics are indicated. As I explain to patients, when you put custom orthotics in your shoes, your feet will now function as optimal feet. If you don’t put custom orthotics in your shoes, your arches are vulnerable to continue collapsing, increasing abnormal loading throughout the body. 2 A years and 308 patients later, I now have conclusive evidence as to what happens to the fhhd when you insert custom orthotics into people’s shoes.
 Fig. 5: Josh's scan vs. Optimal scan
Fig. 5: Josh's scan vs. Optimal scan
There are 5 distinctive biomechanical patterns that all people fall into. Every human has biomechanical faults and imbalances in their feet, knees and leg length. Not one person had perfect feet, aligned knees and level femoral heads. We labeled each pattern as Crooked Man 1-5. Once we knew which Crooked Man they were, specific corrective measures were taken.
I think of Kevin Durant and Klay Thompson who both became injured and will miss a year of their sport because of abnormal loading injuries. If this test had been done on them, the likelihood is very high their injuries might never have occurred.
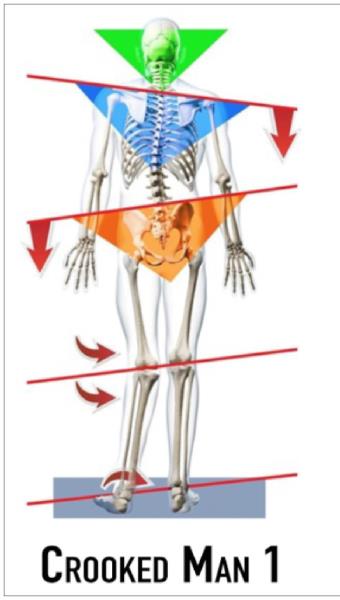 Fig. 6: Crooked Man 1
Fig. 6: Crooked Man 1
This biomechanical model has collapsed arches greater on the side of the low femoral head (Fig. 6). When custom orthotics are put into their shoes, there is a reduction in fhhd. It doesn’t mean the femoral heads become level, it only means they get better as compared to the A-P L-S that was taken barefoot. A heel lift may still be needed.
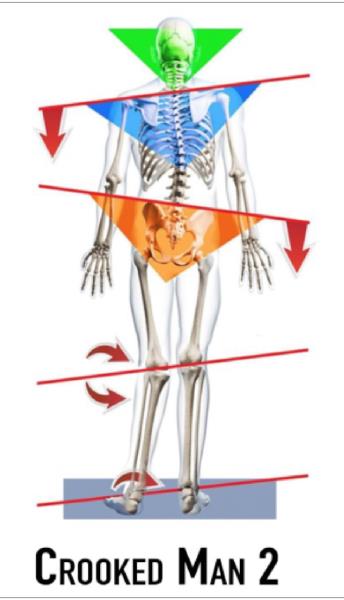 Fig. 7: Crooked Man 2
Fig. 7: Crooked Man 2
This biomechanical model has collapsed arches on the side of the high femoral head (Fig. 7). My theory is that the body continually works to level the femoral heads through all activity, and will even collapse the foot and increase the Q angle on the side of the high femoral head. Once custom orthotics are put into the shoes, the collapsed foot is improved and the Q angle is improved, and the fhhd is now increased. A heel lift will definitely be needed in this case.
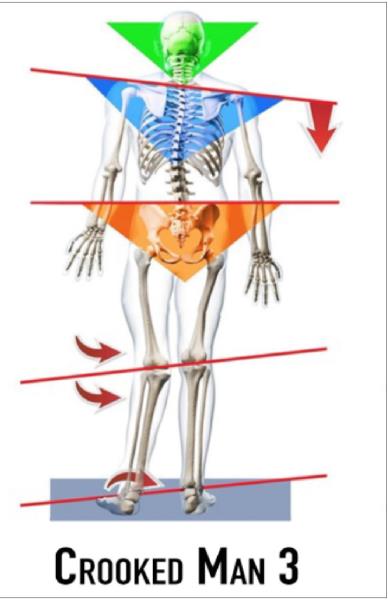 Fig. 8: Crooked Man 3
Fig. 8: Crooked Man 3
This biomechanical model has level femoral heads (less than 3mm difference) on x-ray number one, but has unlevel femoral heads once custom orthotics are put into the shoes (Fig. 8). Again, this is the body’s attempt to level the femoral heads despite the fact the leg lengths are different. Once the feet are corrected and the Q angles aligned, the anatomical leg length becomes exposed.
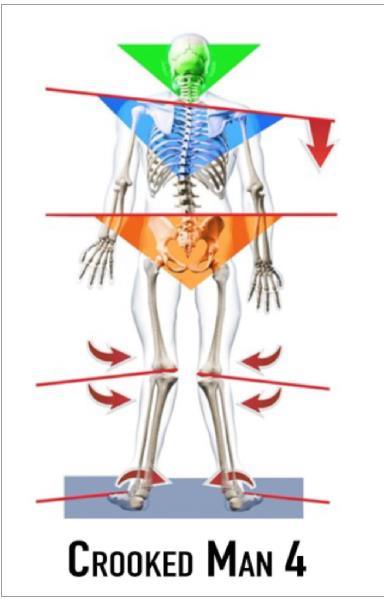 Fig. 9: Crooked Man 4
Fig. 9: Crooked Man 4
This biomechanical model has level femoral heads (less than 3mm difference) on x-ray number one, and also has level femoral heads on x-ray number 2, as the feet have collapsed symmetrically (Fig. 9). Once orthotics are put in the patient’s shoes and the 2nd x-ray is taken, the fhhd is the same as x-ray number 1.
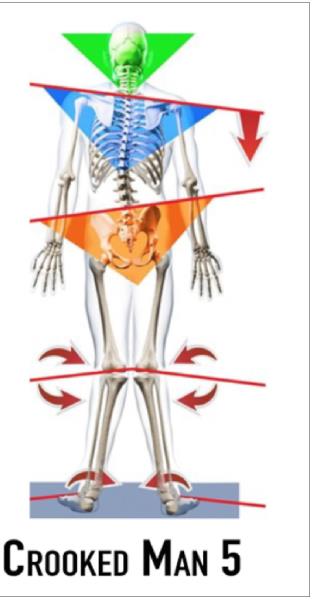 Fig. 10: Crooked Man 5
Fig. 10: Crooked Man 5
This biomechanical model has unlevel femoral head heights (greater than 3mm) and once orthotics are placed in their shoes, they continue to have the same fhhd (Fig. 10).
With identifying which Crooked Man a patient is prior to treatment, the success of any treatment has to go up as abnormal loading throughout the body has been reduced. Long term wellness and returning people back to full activity now becomes a real possibility. If all we do is treat people and never address the inherent abnormal loadings of the body, our treatment results are temporary at best.
Musculoskeletal is the leading cost in healthcare today. All of the leading experts suggest ergonomic evaluations of workstations, improved exercises by our workforce, on-site physical therapy and even meditation. The entire industry is governed by the medical model approach, which is wait for the injury to occur and then react to it. Except, nowhere in this formula is any evaluation of the patient done. No one checks for foot pronations and imbalances, no one checks for increased Q angles, no one looks at fhhd, no one looks at centers of gravity on x-ray, yet we continue spending more money every year on healthcare while quality of life for all of us continues to decline. Joint replacement is a growing industry, Pain Management Centers are everywhere, and 130 people are dying everyday from opioid overdose, with many taking them to reduce musculoskeletal pain in their body.
Chiropractors have the broadest scope of practice in the industry. We know biomechanics. We can look at biomechanics on x-ray and we can order an MRI to determine what impact the abnormal biomechanics has on the discs, the foramen, the meniscus, etc. We can scan the feet and recommend custom orthotics, because if you don’t start at the foundation of any architectural structure, you’ll never solve the ultimate imbalance. We can work nutritionally. We understand rehab. We are one stop shopping, yet so many in our profession want us to follow the medical model, the very model that is the cause of this crisis and leave chiropractic as the low man on the totem pole when we could become the solution to the musculoskeletal crisis.
Hopefully this article will motivate many to adapt a clearer, more solution oriented, opinion and begin looking at the biomechanics of every patient with digital foot scans and digital x-rays. Once our profession informs the world that this is our new model, chiropractic will massively succeed and our schools will overflow with new applicants.
Dr. Tim Maggs, DC, has been in private practice for over 41 years. He has specialized in the diagnosis and treatment of sports injuries throughout his entire career. In 2004, Dr. Maggs recognized the need for improved diagnosis and treatment of sports related injuries in the middle and high school age group. It was at this time he developed the Concerned Parents of Young Athletes™ Program. Dr. Maggs launched his Structural Management® Certification Program in January 2019.
As of July 2019 Dr. Maggs became the proud owner of the Albany Patroons basketball team and is looking forward to an exciting season with them. He is introducing his Structural Management® Program to all teams in the league as it will provide the necessary biomechanical information for each player to prevent and treat injuries more effectively this season and for many more to come. He can be reached at [email protected].
 View Full Issue
View Full Issue