What’s in Your Circle of Concern?
PRACTICE
MANAGEMENT
Ray Foxworth
One of my favorite books is Stephen Covey’s The 7 Habits of Highly Effective People. To me, it isn’t just another business book; its principles are also useful in managing aspects of our practices. For example, when it comes to concerns about risk management, Covey’s explanation of things that are in our “circle of concern” but perhaps outside our “circle of influence” serves as a perfect model of how we can and should focus our efforts on things we can directly control, and look for ways to insure against things we can’t control.
For example, when we look at the risks related to our practices, we see a wide range of things to consider. The following chart reflects things that are within our circle of concern.
POTENTIAL WITHIN OUTSIDE INSURABLE MINIMIZE RISKS CIRCLE OF CIRCLE OF INFLUENCE INFLUENCE RISK SLIPS/FALLS PARTIALLY PARTIALLY OWNER'S BUSINESS YES POLICY (BOP) FIRE PARTIALLY PARTIALLY BOP YES NATURAL NO YES BOP/PARTIALLY PARTIALLY PERILS THEFT PARTIALLY PARTIALLY BOP PARTIALLY COMPLAINTS PARTIALLY PARTIALLY NO YES TO BOARD OF EXAMINERS RANDOM NO YES NO YES AUDITS TRIGGERED YES PARTIALLY NO YES AUDITS
■ ■ While we can insure against the loss, we’d be foolish not to minimize the risks when we can.
From the “potential risks” column, let’s look at how these principles apply and what actions we can take to minimize our risks and protect our practices. Slips and falls are definitely within our circle of concern. We do not want patients sustaining injuries in our offices, but the risk for injuries is both within and outside our circles of influence and fortunately insurable with a proper business owner’s policy (BOP). While we can insure against the loss, we’d be foolish not to minimize the risks when we can. For example, from the parking lot to and from our front door, we have influence over things that would make it less likely someone could slip or fall. Are there cracks or uneven walkways? Perhaps a door threshold or steps that are damaged or too high? Or no railing if there are multiple steps and we practice where there might be snow or ice during the year?
Once in the office, are there power cords that aren’t covered? Is there equipment patients must get on or off where they might be prone to fall? We’ve actually had patients fall off a weight bench while pulling back too far with resistance bands.
■ ^ You can run through the list of potential risks and identify those things that concern you. J J
Thus, it is important to “attend” patients when they are doing rehab, not just for the sake of billing and coding properly, but for safety reasons. Under this category, the things we do not have control over are the patients’ underlying conditions. Are they having difficulty picking up their feet due to foot drop? Do they have an imbalance problem or are they just injuryprone or clumsy?
Another example is fire hazard. If we are in a stand-alone building, we have control over more of the risks than if we practice in a strip center. In our own building, there is little risk from a fire next door. We should instead focus on making sure we don’t have shorted wires on equipment, overloaded outlets, or rugs lying over power cords, to name a few. You get the picture. Fix the things we can fix, and insure against the things we cannot.
You can run through the list of potential risks and identify those things that concern you. Address those within your influence and check your BOP to make sure you’re properly insured for the rest.
Now let’s look at things that are within our circles of concern. Some may be both within and outside our circles of influence. Of most concern are things we typically cannot insure against. Why? Because if we have a problem in these areas, there is no insurance to help cover the potential loss and it can be devastating not only to our practices, but also to us personally.
The first is complaints to our boards of examiners. Complaints can range from annoying to devastating depending on who or what is behind them. While most of our patients are wonderful, we’ve all had patients who, for whatever reason, just can’t be satisfied or are looking for someone to sue. These complaints can range from your making them wait too long (10 minutes) to complaints about your fees or financial policies, particularly if you “demand” they pay their bills or threaten to turn their accounts over to collections. Whether you are right or wrong, it’s at minimum an aggravation to have an unwarranted complaint filed. At worst, it’s a nightmare if the complaint turns into a full-blown investigation should the patient decide to also complain to his or her insurance company or mention the word fraud.
So, how do we deal with these risks? They are partially within and outside our circles of influence. The part outside our circle is the person who is just plain mean, nasty, and prone to complain. The part inside our circle is making sure we train our staff members to identify these people on the front end to make sure they don’t make their way into our
practices. We have the luxury, if not responsibility, to make sure that the people we accept into the practice are a good fit for us and our staffs. We are never required to accept a patient, and we should have some means of identifying those patients up front. You know what I’m talking about. It’s the new patients who call to request an appointment but insist on the phone that they do not want an exam, they sure aren’t going to pay for any X-rays, and they have no intention of making a follow-up visit. They just want you to pop their necks like their last chiropractor did and only charge $5. The moment we bend the rules to accommodate any and every patient who calls is the day we, or at least our staff members, regret. Not accepting these patients is a prime example of how you can minimize complaints that are inside your circle of influence.
Next, make sure your financial policies are simple, compliant, and, more importantly, covered in detail with your patients up front. Why is this so important? Even with great patients, those who aren’t prone to be a problem, uncertainty, or lack of clarity about financial obligations can lead to complaints. In fact, as I’ve often said, one of the top complaints to boards of examiners is not about our clinical care, but about dollars and cents. What I’ve learned recently is that one of the top reasons for malpractice claims is also
■ "Even with great patients, those who aren’t prone to be a problem, uncertainty, or lack of clarity about financial obligations can lead to complaints. JJ
related to our financial policies. How can that be? Atypical scenario is a patient who perhaps didn't get the results he or she expected. When presented with a bill, suddenly you go from being a doctor to being a villain. Some will threaten to sue and others actually do. While you cannot prevent this entirely, you can surely minimize the risk by making sure you cover finances in the beginning so there is no misunderstanding later. The reason this risk is so important to address is that you can’t insure against complaints, so it’s up to you to minimize the risk.
Finally, the greatest area of risk to address is audits. There are two most common types. The first type is random, meaning
an insurance company casts a wide net of post-payment audits and you are just caught up in the net. Then there are triggered audits, meaning there was a direct complaint against you by someone, or something in your billing, coding, documentation, financial policy, or even advertising caused you to be like a player on the Price is Right yelling “Pick me! Pick me!” What’s interesting about these risks is that they are typically the ones we fear the most. They are typically not insurable, which means we have great risk associated with them, and, for the most part, they are the ones we typically have the most control over.
Five of the top things that can lead to triggered audits are dual fee schedules, improper time-of-service discounts, inducement, and anti-kickback and false claims violations. One of the most common, and the one that is easiest to fix, is the dual fee schedule. Dual fee schedules can lead to audits when there are state rules and regulations that prohibit charging more to insurance carriers than you do to patients paying cash. While this is commonplace, dual fee schedules can violate regulations and the terms of many provider agreements. Quite frankly, it also doesn't look right to patients when they know you are charging more to insurance. If you don’t believe that, you should have been with me when one of my patients told me she reported me to the attorney general for charging more to her auto carrier than I charged to her when she was private pay. Did I? Yes. Back then it was commonly done and it wasn’t against
^Most importantly, make sure every patient gets a financial report of findings that covers your policy in addition to their clinical report of findings. 5 J
my state regulations. However, the perception was horrible and she accused me of being a bad guy who was ripping off insurance companies resulting in rates she couldn’t afford. This risk can be easily minimized by making sure you have one fee schedule, and the only time you offer discounts is if you are part of the patients’ in-network health plans; treating patients with a mandated fee schedule (such as Medicare, Medicaid, workers’ comp, or personal injury); if patients are members of a discount medical plan; or if patients meet your financial hardship policy.
If we know that our financial policies are one of the top complaints to boards of examiners, insurance companies, and malpractice carriers, and we typically cannot insure against that risk, then it makes sense for us to minimize this risk by having financial policies that are simple, compliant, and profitable. Most importantly, make sure every patient gets a financial report of findings that covers your policy in addition to their clinical report of findings. Don’t let things such as dual fee schedules, improper time-of-service discounts, inducements, and anti-kickback and false-claims act violations that are in your circle of concern and your circle of influence continue to put you at risk. You have direct control over them. Stop yelling “pick me” and practice with peace of mind.
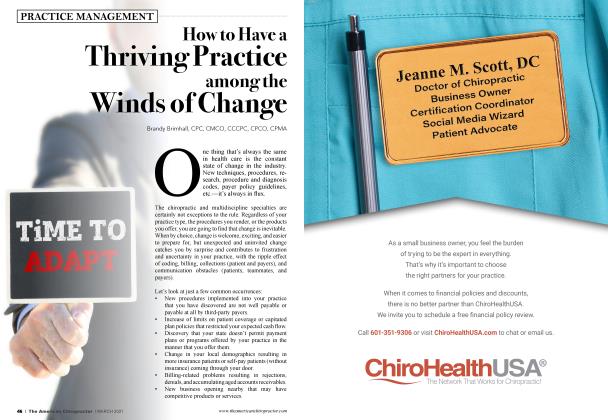
Dr. Ray Foxworth is a certified medical compliance specialist and president of ChiroHealthUSA. As a practicing chiropractor, he remains “in the trenches” facing challenges with billing, coding, documentation, and compliance. To request a five one-page financial policy, send an e-mail to infofichirohealthusa.com. If you ’d like more information on practicing'with peace of mind when it comes to your financial policies, go to www. chirohealthusa. com
 View Full Issue
View Full Issue